Cohen Monitor Report Hadix v Johnson Mi Prisoner Health Care Sept 2005
Download original document:
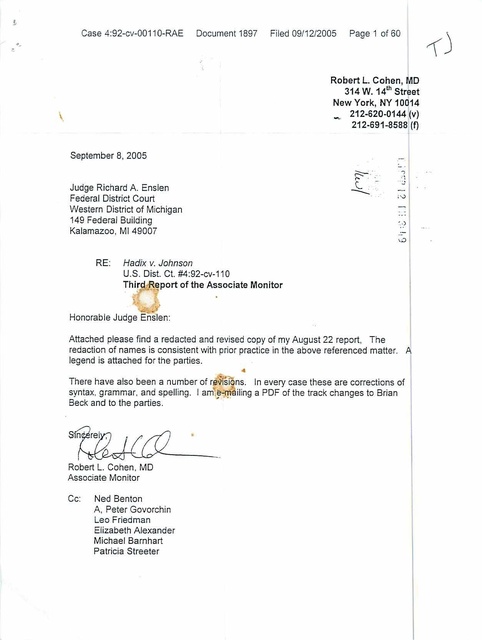
Document text
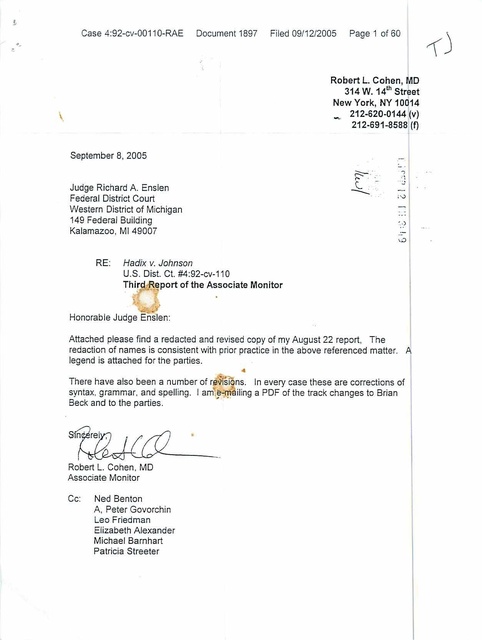
Document text
This text is machine-read, and may contain errors. Check the original document to verify accuracy.
Case 4:92-cv-0011 O-RAE Documenl1897 Filed 09/12/2005 Page 1 of 60 -Robert L. Cohen, MD 314 W. 14~ Street New York, NY 10014 -. 212-620-0144 I(v) 212-691 -8588 (f) Seplember 8, 2005 o :~ , ." Judge Richard A. Enslen Federal District Court Weste rn District of Michigan 149 Federal Building Kalamazoo, MI 49007 RE: , oJ ..) Hadix v. Johnson U.S. Di st. Ct. #4:92-cv-110 Third ~.Report of the Associate Monitor Honorable Judge Enslen: Attached please find a redacted and revised copy of my August 22 report , The redaction of names is consistent with prior practice in the above referenced matter. A legend is attached for the parties. " • There have also been a number of r~l)is i ns. In every case these are co rrections of syntax, grammar, and spelling. I am .~i!1 iling a PDF of the track changes 10 Brian Beck and to the parties. Robert L. Cohen. MD Associate Monitor Cc: Ned Benton A, Peter Govorchin Leo Friedman Elizabeth Alexander Michael Ba rn ha rt Patricia Streete r • THlRD REPORT OF THE ASSOCIATE MONITOR Hadi.:" v. Joiznson ROB ERT L. COHEN, I\1D September 8, 2005 TABLE OF CONTENTS Report Page INTRODUCTION . . . .... . . . . . ......... .. . . ...... . . . ..................... I AD1v!INISTRA nON .. . . . .. . ......... . . . . .... . .. . .... . .... .. .......... 2 MEDfCAL SERVICE PROVIDERS .... .. . ................... . ... .. ........ 3 INT.A.KE .................................. . .....•.... .. ...... .... ..... 3 PRISONER HEALTH CARE CO-PAyMENT .. . . . . . . . . ...... . ...... . ....... 4 CHROl\1JC CARE ..... . ......... . .. . ........ . ..... • .......... . . . ... ..... 4 DIALySIS ... ... . ................ . ...... ... . . .... . ...... . .. . .•.... ... . . 5 PHARMACY . .. ... ... . . . ..... . . . .... ...... .. . . ... . .•.... . ...• . • . •.. ... 7 MEDICAL RECORDS ... . . • .. ...... . .. ... . ........ . .. •. . . . .. . ....... .... 7 SPECIALTY CARE ........ .... . . .. . .. . .. .. .. . .. . . . . . . .. . .• .. . .. . . .. . ... 9 INTECTIOUS DfSEASES . . . . . . .. . . • . . . . . . . . . . . . . . • . .. . .. . . . . . . . . . . . . . . . . 10 SEGREGATJON . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . .. . .. . . . . . . . . . . . . . . .. II C-UNIT . ..... .... . ........... .. .. . .. . ........ . . . . . . . . . . . .. ..... ...... 12 DUANE WATERS HOSPITAL .. .. . .. . . . . ... . . .... .. • . •. ................ 14 CASE REVIEWS ... . . . . . . . . ..•..... ............ Patient 1 ........ . ..... .... .. . ................. . ...... ..... . . .. . -Comment on Patient I .......... . .. .. . . . . . .... . . ... .. ... . .. .. .. .... Patient 2 ...... . . . .. . ..... .. .. .. . . .. . ....... . .... . .. .... .. . . .. . . . -Comment on Patient 2 . ..... .. . .. . . . . .. . .... . .. .. . .. ... .. . . . . ...... Patient 3 .. ........ . .. . . . .... .... .. .............. ... ......... . -Comment on Patient 3 .......... . ..... . .... . .. . .. . . . . .. . . . . . .. . ... . 16 16 19 20 23 ?' -.) 29 Patient 4 ....................................................... 30 -Comment on Patient 4 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. 31 Patient 5 ....................................................... 32 -Comment on Patient 5 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. 42 Patient 6 ....................................................... 143 -Comment on Patient 6 ............................................ I 44 Patient 7 ....................................................... 44 -Comment on Patient 7 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. 46 Patient 8 ....................................................... 47 -Comment on Patient 8 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. 50 Patient 9 ........................................................ 51 -Comment on Patient 9 ............................................ J 52 CONCLUSIONS ...................................................... 53 RECOMMENDATIONS ................................................. 55 . Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 31d Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert l. Cohen. MD Page 2 of 60 September 8, 2005 page #1 INTRODUCTION This is the third report of the Associate Monitor on Health Care in the Hadlx matter. This report is based upon my tours of the facilities, interviews with staff and prisoners, review of medical records, review of documents, and meetings with counsel to the parties. It covers my review of medical care for the first seven months of 2005. My last visit to the facility was on August 4,2005. In response to the Second Report (January 11, 2005), a series of conversations and meetings, chaired by the Associate Monitor, were held to review serious problems in the delivery of medical care in the Jackson facilities. New policies were developed in the following areas: Criteria for charging co-payments Chronic Care in the C-Unit Care in the JMF Segregation Unit Dialysis - Suicide prevention, vascular access Inter-institutional Transfers This review of will cover those issues, as well as the following subjects: Staffing, supervision, and organizational issues at Duane Waters Hospital. Limitation in access to specialty care Failure to recognize and treat life threatening conditions Medical Records Pharmacy Infection Control The report will conclude with a number of specific recommendations, some of which should be Implemented as soon as possible. Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 Page 3 of 60 111 3 Report of the Associate Monitor Revised and Redacted Had'/X v. Johnson Robert L. Cohen. MD September 8, 2005 Page #2 ADMINISTRATION There has been significant instability in the Correctional Medical Services (CMS) administration of their MDOC contract at the Hadix facilities. In response to concerns about Inadequate supervision of MSP staff expressed in the First Report of the Associate Monitor, CMS hired Dr. Austin as Associate Medical • Director for CMS In the Jackson Region. He assumed this position on September 15, 2004. He remained in the position for approximately six months, when he moved to Texas. During his tenure Dr. Austin did not establish an effective system of supervision or monitoring of CMS staff in the Hadix facilities. Dr. Mathai was apPOinted Medical Director in April, 2005. Based upon her initial efforts, she appears to be an excellent choice for this pOSition. She has had significant clinical experience at Duane Waters Hospital (OWH) as well as SMT. Dr. Gregory Naylor, the Regional Medical Director for the Jackson Medical Region, announced his resignation in July, and will retire in August No replacement has yet been identified, according to Dr. Pramstaller. Dr. Naylor was not successful in using his position as Regional Medical Director to improve the quality of supervision of the clinical staff, to support continuing education, or to develop speCific initiatives to improve the quality of care. It is noteworthy that although he had been the Medical Director of DWH, the dysfunctional MSP situation at C-Unit and at DWH developed during his tenure. As I suggested in my first report, MOOC should use the opportunity of his reSignation to define the role of the MDOC Regional Medical Director of the Jackson Complex. This position should provide clinical leadership to the medical program of the Jackson Complex, should monitor CMS performance. and should provide clinical support to the pharmacy and nursing functions. The Regional Medical Director should also organize a continuing education program for the staff of the Jackson Complex. ' Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 3n1 Report of the Associate Monitor Ravlsed and Redacted Hadix v. Johnson Robert L Cohen. MD Page 4 of 60 September 8. 2005 Page #3 MEDICAL SERVICE PROVIDERS An effective program of MSP supervision by CMS has not yet been developed. There was no clinical supervision of MSP staff at C-Unit or Duane Waters Hospital. which has been staffed by Dr. Fuller's Emergency group. Dr. Mathai has been assigned this supervisory responsibility. At the present time CMS is not providing adequate medical staff at the Hadix facilities to support the enhanced cUnical function created by the addition of the dialysis program and the establishment of the C-Unlt program. Additionally, the role of Duane Waters Hospital has changed, becoming more clinically intense, while the medical staffing of the Hospital has actually decreased. When new MSP's are assigned by CMS to the Hadix facilities, they are not trained in SERAPIS (CMS' Electronic Medical Record System, purchased by MOOC), and are unable to enter their notes, pharmacy orders. and laboratory orders into the SERAPIS system. This creates significant problems in the medical records, as will be described below. Some CMS MSP's work in multiple facilities, and they are not able to use the SERAPIS system in more than one facility. According to Sharon von Hom, this is a problem with the MOOC system. not SERAPIS. This is a critical deficiency and needs to be resolved urgently. At the present time. because of inadequate physician staffing. Dr. Mathai is required to work as a staff phYSician to fill in for scheduled vacancies. Staff tumover continues at a significant level for CMS physicians. and recruitment for adequate coverage at C-Unit and OWH has been unsuccessful. fNTAKE - According to Mr. Govorchin's August 16 th letter to Ms. Streeter. MDOC has adopted a new process for intake medical transfers. Prisoners transferred into Hadix facilities will have all of their prescribed medication noted through one of three mechanisms: "printing the list from SERAPIS, noting the list . Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 Page 5 of 60 111 3 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD September 8, 2005 PageM in the progress notes or noting the medications on the transfer screen." Medical reviews of Inter-institutional transfers are a fundamental function of the Hadix medical system. There should be a speCific, defined procedure for medical review and evaluation of newly transferred prisoners. There should not be a menu of options. Special attention must be paid to the medical needs of prisoners transferred directly into the Segregation Unit at JMF. Several cases are described below where these patients' medical needs were neglected because of their transfer directly into JMF segregation. PRISONER HEALTH CARE CO-PAYMENT A new procedure for assessing co-payments was promulgated on April 15, 2005 to assure that patients with significant ongoing or chronic medical problems would not be denied access to care because of the co-payment system. Although no standardized audits of this new procedure have been implemented, according to a memorandum from Kathy E. Blyd to Barbara Hladki dated June 21, 2005, the number of co-payments assessed in May 2005 compared with February 2005 has decreased by two thirds. CHRONIC CARE There is a functioning chronic care system present in JMF, excluding patients with chronic illness housed in segregation. The SMT chronic care program is functioning. Each of these programs would be substantially enhanced if the Nursing chronic care function were related to the MSP chronic care encounter. Rather than having an essentially non-clinical encounter every six months, Nursing support of chronic care should take place a week or two before each scheduled MSP visit. and involve chart organization. assuring that necessary laboratory and diagnostic studies will be available at the scheduled Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 3n1 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen, MD Page 6 of 60 September 8, 2005 Page #5 MSP chronic care clinic. reviewing and assuring medication compliance and continuity, and patient teaching. The chronic care program is not operational for prisoners housed in CUnit and in DWH. although a commitment to develop a chronic care program In C-Unit has been announced. DIALYSIS Three audits of the Dialysis unit were provided to me, for May. June. and July, 2005. According to Barbara Hladki. the first two audits were conducted without benefit of the dialysis record. The results of the May and June audits. conducted by Dr. Naylor and Dr. Hutchinson were very positive. but they were not based on clinical data. The second audit provided to me. performed in July. 2005. was much more problematic, because it was based on actual review of medical records. It showed that half of the ten patients reviewed had significant hypertension postdialysis. without any urgent treatment response. Additionally, for those patients with poorly controlled "steady state- hypertension, 50% (5/10) were not addressed by the nephrologists. It also showed that the indicator of dialysis effectiveness, the "urea reduction ratio" was abnormal in SO % of the cases (S/10) reviewed, and that there was no response by the nephrologists in 40% (4/10) of these cases. The audit tool looks at a indicators. Dr. Middlebrook, the nephrologists, received 25% of his positive score for writing a monthly note. and for obtaining the "urea reduction ratio." This gives Dr. Middlebrook too much credit for just "showing up." Writing a note each month which fails to address major clinical needs in at least half of the patients reviewed should not be given "full credit.· The results of the July audit were to be addressed by Dr. Mathai at a special meeting with Dr. Middlebrook, the nephrologist, on July 22, 2005. That meeting was cancelled by Dr. Middlebrook. As of August 4, Dr. Middlebrook had Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 atd Report of the Associate Monitor Revised and Redacted Hadlx v. Johnson Robert l. Cohen. MQ Page 7 of 60 September 8, 2005 Page #8 not met with Dr. Mathai to discuss these issues. Although Mr. Govorchin, in his August 16 letter promised increased availability of Dr. Middlebrook to the Dialysis program at JMF, I have not yet seen any evidence of this increased commitment. There is no SERAPIS terminal in the dialysis unit Laboratory studies which are ordered through SERAPIS are not being filed as paper reports in the medical records. According to the July Dialysis Audit: ~SERAPIS availability for the Nephrologists and the Unit Manager (of the dialysis unit) is being pursued. Instructions will be reiterated to ensure that the Nephrologists monthly notes are in the DOC health record and that a list of current medications will be provided from SERAPIS or Tiny Terms (the pharmacy computer system, which is not linked to SERAPIS) to the (?nephrologists) at the time the monthly notes are written." An additional problem discussed in the Associate Monitor's Second Report, and covered in Mr. Govorchin's August 16 letter, concerned elective and emergency access to appropriate vascular surgery conSUltation. This situation is still substantially un-resolved. On August 4,2005, a number of the dialysis patients were being held at Detroit Receiving Hospital because CMS no longer has access to a number of the surgeons who had been performing vascular access procedures at Foote Hospital Dr. Camann, an experienced internist, had been given the responsibility for all of the dialysis patients at JMF. Dr. Camann recently resigned his position. Dr. Faghihnia has been assigned this responsibility. Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 31'11 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen, MD Page 8 of 60 September 8, 2005 Page#? PHARMACY The bi-monthly facility audits suggest that there are approximately forty medication kites submitted each month (excluding RGC) because of problems with renewals of medications. Barbara Hladki Is conducting a study of these medication kites but has not completed it. I reviewed the system for medication renewals in JMF in July, and was impressed with the significant improvements which had taken place. A significant miSSing piece in the system is the integration of SERAPIS into the pharmacy system. The pharmacy program is also missing drug interaction identification software which includes HIV medications. This was apparent in one of the cases reviewed below. MEDICAL RECORDS There are two separate medical record systems in operation at the Hadix facilities, a paper record, and a computerized record. The computerized medical record, the SERAPIS system, is a CMS product which has been modified for use by the MDOC. New CMS physician and mid-level providers begin working in Hadix facilities before they have been trained in the use of the SERAPIS system. They are therefore unable to use the system, and write their notes and orders in the medical record, CMS practitioners who work in more than one of the Hadix facilities are not permitted to log in to the SERAPIS system at both facilities. There is no SERAPIS terminal in the JMF Segregation Unit. There is no SERAPIS terminal in the Dialysis Unit. Case 4:92-cv-00110-RAE Document 1897 Filed 09/12/2005 Page 9 of 60 111 3 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD September 8, 2005 Page #8 Medications ordered on paper which are faxed or delivered to the pharmacy are not included in the SERAPIS system. All medications are entered, by hand, into the MTiny Terms" pharmacy system, but there is no interface between "Tiny Terms" and SERAPIS, and no interface is planned. Laboratory tests which are ordered in SERAPIS are electronically transferred from the Garcia Lab directly into the computer system, and are not printed out for the medical record. Laboratory studies not ordered through SERAPIS are not available in the computer system, but they are printed out and are present in the paper medical record. The Emergency Room at Duane Waters Hospital does not have a SERAPIS terminal, and clinicians there did not have access to the SERAPIS medical record. There is no plan to implement SERAPIS in Duane Waters. Similarly, there are no SERAPIS terminals at C-Unlt. Physicians, including those working in the Dialysis Unit, C Unit, DWH and the DWH Emergency room must review a patient's paper medical record without access to SERAPIS. These physicians do not have access to the results of laboratory studies which were ordered In SERAPIS. At the present time, the MSP and nursing staff at SMT, JMF, and RGC use both systems. Because of the concurrent use of two systems, the medical records are voluminous, difficult to use, and are not in chronological order. The medical records are not in chronological order because the SERAPIS notes are printed out individually, often a few lines on an entire page, sometimes four or five printed pages, while handwritten notes are written sequentially on progress note pages in the paper medical record. There must be a unified medical records system. The SERAPIS system may be adequate, and if it is used, it must have a direct interface/order entry function into the pharmacy system so that all medication information will be current and correct. All laboratory data must be present in SERAPIS, whether Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 3111 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 10 of 60 September 8, 2005 Page #9 ordered in SERAPIS or not. All clinical areas must have functioning SERAPIS terminals. Clinicians who work in more than one facility must be able to enter data and review data in each of the facilities in which they work. SPECIALTV CARE There is a continuing serious problem with access to specialty care for patients in the Hadix facilities. Although all consults are logged by CMS into their computer system, CMS has not been helpful in providing information to MDOC about delays in providing specialty care, and through 2005, did not oversee the quality of its staff follow-up of these issues. Extraordinary delays in the care of very sick patients with cancer, renal failure, AIDS have occurred over the past year. Barbara Hladki, the Regional Administrator, has implemented a computerized system to allow MOOC to track the access of Hadix class members to conSUltation with CMS speCialists and for specialized procedures. According the "Offsite Specialty Log Summary" compiled for the first six months of 2005, 41 % of all completed initial consults, and 45% of all completed follow-up conSUltations were not completed within the requested time frame. This is unacceptable, and results in significant delays in the diagnosis and management of serious, as well as life threatening illnesses. The MSP 30 day review of pending consultations is a failed system, Using data generated by the MOOe specialty care computer system, Barbara Hladki, Dr. Mathai. and Dr. Naylor (during his tenure) are reviewing all consults which have not been scheduled. or have not yet take place within the requested time frame. They are meeting every two weeks in each facility with the MSP staff to review each of these consults. This is a good system, which hopefully will result in fewer and fewer consults occurring past their scheduled dates. MSP staff have an obligation to track their consult requests, and to assure that patients Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 3rd Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 11 0160 I September 8, 2005 Page #10 requiring specialty care and special diagnostic procedures receive them in an appropriate time frame. In some cases, particularly involving the PA and NP staff, I have noticed a tremendous effort by these practitioners to obtain urgent consultations for their patients. Unfortunately, their efforts were often thwarted by the CMS system. At the present time eMS specialists fill out a handwritten consultation form at the time of their evaluation, and then dictate a formal consultation, which is typed and sent to the facilities. There is often a substantial delay in receipt of the typed dictations, yet it is the policy of CMS' MSP's not to review hand written consultation requests. It is also the policy of CMS not to honor their own specialist's requests for diagnostic testing until the typed consult is received. This system is designed to delay necessary specialty consultations, and is hazardous to the health of patients. Consultations are routinely not viewed by MSP's until after typed consult received, even though the written note often has important information requiring action by the MSP. MSP's should review these handwritten consultations when they are available. When a specialist believes that an urgent treatment, diagnostic test, or additional consultation is indicated, a phone call should be made directly to the referring MSP. INFECTIOUS DISEASES Although there have been periods in the past year when there were significant delays in access to HIV specialty care, additional infectious disease consultant time has been made available to care for prisoners with HIV and Hepatitis C infection. The Michigan legislature has been considering limiting funding for treatment of Hepatitis C infection in the MDOC. It is not yet clear how proposed budgetary restrictions on Hepatitis C treatment will affect the care of patients in the Hadix facilities who require treatment for this infection. Case 4:92-cv-00 11 O-RAE Document 1897 Filed 09/1212005 ~ Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L Cohen. MD Page 12 of 60 September 8, 2005 Page #11 On April 13, 2005, I reviewed the MRSA control program for the Hadix facilities. At that time I noted that there was no functioning tracking system for patients with MRSA infection. Culture reports were collected by the Infection Control Nurse, but no case investigations were performed, no infection control poliCies regarding isolation/quarantine were in effect, and no epidemiologic investigation of the cases at the Hadix facilities had been performed. I noted that there were three clusters of cases at three of the Hadix facilities: C-Unit, the Dialysis Unit, and at DWH hospital. I informed the medical leadership of the facilities of my findings. On April 14, 2005, Richard O. Russell, Administrator of the Bureau of Health Care Services for the MoOC issued a Memorandum on MRSA infection. The first line of the memorandum states: "Effective Immeciiately, all prisoners with a documented culture positive for MRSA must be quarantined (Bold In original)." Also issued on April 14, 2005 was a three page set of guidelines on the correctional and nursing management of MRSA infection. These guidelines call for daily nursing visits for patients quarantined for MRSA infection. They also Include guidelines for reporting and epidemiologic investigation. It is noteworthy that Patient #8, whose care is described below, was being treated for MRSA. He was segregated in JMF, but not quarantined. Except for his first day at JMF, he had no medical and no nursing visits to assess his purulent wound during his three week stay in Segregation at JMC. Mr. Russell's guidelines required daily nursing visits. Patient #8 died of neglect. MRSA, and gastre-intestinal bleeding. SEGREGATION In my January report I identified serious problems with access to medical care for prisoners in Segregation. MoOC developed new procedures to attempt to address these problems. These procedures specifically involve a monthly Case 4:92-cv-00110-RAE Document 1897 Filed 09/12/2005 m 3 Report of the Associate Monitor Revised and Redacted Hadbc v. Johnson Robert L. Cohen. MO Page 13 of 60 September 8, 2005 Page #12 chart review of half of the patients enrolled in chronic care clinics. A nurse was assigned specifically to the Segregation Unit. Based upon my review of patients in segregation in April and May, medical care for these patients is still very problematic. Patients with critical life threatening illnesses were completely ignored, treated inadequately. Patients with extreme pain and massive weight loss are not properly evaluated and treated. There seem to be many psychotic inmates in segregation, and they have significant medical problems but have difficulty expressing their medical needs. There is a significant problem with provider continuity. C UNIT The C-Unit was opened in the spring of 2003, and it currently houses approximately 59 chronically ill men who are too sick to live in general prison population. These prisoners often have multiple chronic illnesses, including AIDS, Hepatitis C, as well as decompensated pulmonary and cardiac illnesses. Medical staffing for this population was provided by CMS through a subcontract with Dr. Fuller, who has been providing medical care to Dwayne Waters Hospital and its Emergency Room. No additional staff medical service providers were hired to care for this chronically ill prisoner population. The system of chronic care dinics, with regular structured nursing and physician evaluation according to defined protocols was not extended to this population. Care in the C- Unit has been chaotic because of significant understaffing. From the beginning of 2005, and perhaps much earlier, it was apparent that eMS was unable to provide adequate medical coverage for Dwayne \lYater's Hospital and C unit. CMS has contracted with Emergency Medical Consultants, a corporation run by Dr. Fuller, to provide physician and mid-level practitioner staff for C Unit, Dwayne Waters Hospital in-patient units. as well as 24 hour coverage of the Dwayne Waters Hospital Emergency Room. I Case 4:92-cv-00110-RAE Document 1897 Filed 09/1212005 3111 Report of the Associate Monitor Revised and Redacted Had/x v. Johnson Robert l. Cohen. MD Page 14 of 60 September e, 2005 Page #13 Although the crisis in MSP staffing and severe deficiencies in quality of care was acknowledged by MOOC staff in March, 2005, the actual full time medical staff available to C-Unit, OWH and the DWH ER decreased this spring, exacerbating a dangerous situation. The Regional Medical Director for the Jackson Region, although based at Dwayne Waters Hospital, did not recognize these serious ongoing problems, and made no effort to identify the source of the problems or to correct them. The CMS Deputy Medical Director, Dr. Austin, although responsible for supervising the MSP staff in the Hadix Facilities, did not supervise the C-Unit or DWH staff. The Nursing administrators at DWH and CUnit told me that were aware of the problems, and agreed that the problems had serious implications for patient care, but they did not have any solutions. They viewed the MSP availability as so strained that they did not think it was possible to expect them to write notes or to respond to nursing requests for patient evaluations. The Medical Director did nothing to resolve these problems. It was not until June 21, 2005, in a memorandum from Lisa Sweet-Brown, that CMS announced that: "Correctional Medical Services has made the decision to provide the Hospltalist and primary care at Duane Waters Hospital and C-Unit Directly and transfer this service responsibility from Emergency Medical ConSUltants (i.e. Dr. Fuller). We will continue to utilize Emer.gency Medical Consultants for emergency room coverage at Duane Waters Hospital only.... This transition will be phased in beginning July 5.2005." As of August. 2005, no new staff have been hired. Dr. Mathai is assigned to provide direct care at C-Unit twice a week. According to Barbara Hladki, CMS plans to hire 3.2 full time equivalent (FTE) MSP staff for DWH and C Unit. CMS will guarantee at least two full time MSP's Monday through Friday at C-Unit and for inpatients at DWH. They plan to add an additional four hours of coverage on weekends. Should this staffing be achieved, it will represent more than a doubling of current DWH/C-Unit staffing. It is extremely distressing that adequate additional staffing was not provided when C- Case 4:92-cv-00 11 O-RAE Document 1897 Filed 09/12/2005 Page 15 of 60 Rt 3 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson .Robert L. Cohen. MO September 8. 2005 page #14 Unit. a 59 bed unit with extremely high medical utilization, was opened two years ago. DUANE WATERS HOSPITAL There has been a dramatic change in the role and function of Duane Waters Hospital. In recent years it had served four functions: 1. Acute post-operative care, for the patients receiving simple surgeries at DWH, or re-covering post op from surgeries at Foote or other Hospital. 2. Acute and chronic care for severely mentally ill prisoners. This function has been transferred to other MOOC facilities. 3. It also has a chronic care function, linked closely to C-Unit. which it provides for the entire MOOC system. OWH can take patients of all security classifications, while C-Unit appears to have exclusions for patients In Segregation status. These are patients with significant physical disabilities. sometimes orthopedic, usually involving significant medical problems which limit their activities of daily living. These patients are sometimes in a terminal status 4. Acute hospital care, for patients with acute medical problems requiring relatively intensive nursing and medical care, such as severe asthma, pneumonia, gastroenteritis. infections requiring intravenous antibiotics. These patients are too sick to be housed in general population. This is a rapidly growing population, and OWH has limited capacity for these patients. Almost all acutely ill patients from the Hadix facilities are sent to OWH for emergency evaluation. DWH ER medical staff must then elect to send them to Foote for further evaluation and diagnostic testing, back to their housing areas, or admit them for acute care. Because of insufficient capacity at DWH. there is no ability to maintain a group of available beds at DWH for acutely ill medical patients from the Hadix facilities. Case 4:92-cv-0011 O-RAE Document 1897 Filed 09112/2005 3rd Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 16 of 60 September 8, 2005 Page #15 This is a necessary function for a population of more than 5000 prisoners. Theoretically these patients can be sent to Foote Hospital, but review of the cases below shows that Foote regularly returns acutely ill patients to DWH, even when they are aware that no DWH hospital beds are available. The lack of acute beds at DWH. as well as the lack of medical staff at DWH has resulted in a situation where MSP staff at DWH are forced to send acutely patients back to their housing areas for ongoing treatment of medical problems which are beyond the capability of the SMT or JMF medical staff. Alternatively, when they are required to admit acutely ill patients, they often admit them as "chronic patients," which means that the patients will only be seen monthly by MSP staff. I reviewed the care of a patient (Patiente #10) with bilateral pneumonia and a persistent elevation of temperature who had failed a course of oral antibiotics. The patient was sent to the DWH Emergency Room for care, and was sent back to their housing area with a recommendation for an antibiotic change. The patient was much too ill to be care for at JMF, needed close nursing coverage and intravenous antibiotics. The patient decompensated further, was eventually hospitalized at Foote, and died. In response to these problems, several changes have been proposed, and some implemented. Patients are no longer admitted to DWH Hospital as "chronic." All patients are initially admitted as acute, and are treated as acute patients for at least 72 hours, because their classification has changed. There has been a commitment to increase staffing for C-unit and for the Hospital beds at DWH, expressed to me for the past four months, but the staffing has not increased, in fact during much of the period it decreased. The responsibility for supervision of the "Hospltalist (non-emergency room staff)" MSP's at DWH has been taken away from the Fuller Emergency Medicine group and will be assumed directly by the eMS Deputy Medical Director, Dr. Mathai. Case 4:92~cv-0011 O~RAE Document 1897 Filed 09/1212005 Page 17 of 60 111 3 Report of the Associate Monitor Rav/sed and Redacted Hadix v. Johnson Robert L. Cohen. MO September 8, 2005 Page #16 CASE REVIEWS Following are a series of case reviews which are representative of the serious problems that I found in reviewing the medical records of prisoners at DWH, JMF Segregation, and the charts of prisoners who died while in the Hadix facilities. Patient #1 Patient #1 has AIDS. He also has chronic hepatitis B and chronic hepatitis C. He also suffered from s;cca syndrome, a condition of extreme dryness of the mouth and esophagus, causing chronic pain and difficulty in swallowing. He was housed at JMF Segregation. He had been prescribed Invirase 1000mg twice a day, Kaletra 3 tabs twice a day, Viread (tenofovir) 300 mg once a day, and Videx EC 400 mg twice a day, beginning in 2003. He is always described as cachectic. On October 29, 2003, when he was seen by Dr. Crane, one of the HIV speCialists, he weighed 123 pounds, up from 121 in August, 2003. On February 13 Dr. Faghihnia saw Patient #1 in the 10 chronic care clinic. He noted that he weighed 108 pounds, and had lost 10 pounds, almost 10% of his body weight. He found him to be stable, and scheduled a three month followup. On February 27, 2004, a lipase level was measured and was elevated at 83, an abnormal elevation. A week later he was seen again by Dr. Crane Patient #1 complained of increased difficulty swallowing his food because of his lack of saliva, with the pain descending into his esophagus. At this visit he weighed 110 pounds, thirteen pounds less than four months before. He was markedly malnourished. Dr. Crane wrote: "Despite his special dietary orders, he Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 3n1 Report of the Associate Monitor Revised and Redacted Had/x v. Johnson Robert l. Coben. MD Page 18 of 60 September 8, 2005 Page #17 has not been consistently provided with an adequate mechanical diet so that he can eat properly...... his level 4 segregation has resulted in him falling behind in terms of his nutrition. This patient is now seriously mal-nourished. M Based on Dr. Crane's assessment, Dr. Camann, Patient #1'5 physician at JMF, worked to get him admitted to DWH to assure that he would get appropriate nutritional support. On May 5, 2004 Dr. Crane again examined Patient #1. He noted that "he is a chronically ill appearing, skeletal appearing man .... He weighs 112 pounds in chains." On August 8,2004, his weight was recorded as "107, in chains." There was no notation as to whether these were the same chains which bound him three months before, nor an indication of the weight ofthe chains. His Tcells were 170, down from 220 on 1/16/04. Dr. Crane noted "Despite his efforts, he is not transferred to a chronic care unit and continues in a level 5 segregated unit On September 24, 2004, Dr. Camann saw the patient. In response to the patient's complaint of persistent severe epigastric pain, Dr. Camann ordered an UGI and Small bowel follow thru (X-ray contrast study). On October 22, 2004, Dr. Camann again requested this study. The study was performed and reported as normal. On November 10, 2004, Dr. Crane saw the patient in the Infectious Disease Clinic. His weight was recorded as "116 (with) Iron." Patient #1 told Dr. Crane that for the past three months he has had significant abdominal pain "which occurs during meals and lasts anywhere from an our to overnight after eating." An appOintment scheduled for December 15, 2004 was cancelled because the patient was in Segregation. In their April report on Segregation Drs. Naylo'r and Austin note that "Patient was unable to keep apPOintment to Infectious Disease on December 15, 2004, but was followed by Dr. Camann appropriately and is currently at DWH. The missed Infectious Disease appointment does not Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 31d Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 19 of 60 September 8, 2005 Page #18 appear to have hastened the patlenfs admission to DWH.· Their observation is correct, since Dr. Camann and Dr. Crane had been trying to get Patient #1 into DWH for almost a year. Unfortunately, on January 7, 2005, when Patient #1 was finally admitted to DWH he was directly admitted as a "chronic patient." This meant that he would be seen by an MSP on a monthly basis, only. The consequences of "chronic" status quickly became apparent. The First MSP note was written on January 7,2005. Dr. Howse wrote: "Pt. is here for End Stage HIV with wasting syndrome, transferred at request of Dr. Camann for failure to thrive on salvage therapy. Pt. is alert, able to sit up, verbally coherent + temporal wasting." No other examination took place. No review of his medications or of his active medical problems, which were weight loss, HIV infection, sieea syndrome, abdominal pain, and chronic hepatitis. No effort was made to address any of his multiple painful and life threatening medical problems. Four days later, on January 14, 2005, Patient #1 reported "I've had this rash for at least 2 days. It bums and itches." The nurse noticed raised red areas in the left lower quad and flank. She wrote "Note placed on Drs. Sheet about rash." The doctor, who was supposed to read the "Drs. Sheet" on a daily basis and respond never came to see the patient. Four days later, he again complained about the rash, which was itching and buming, raised and reddened. Then nurse again requested the doctor to see the patient and Dr. Howse came and saw that Patient #1 had a vesicular rash characteristic of Herpes Zoster. This is an extremely painful rash, and can be particularly dangerous in an immunocomprornised patient. Dr. Howse treated Patient #1 with intravenous acyclovir. On January 24, one of Patient #1 's teeth crumbled, and he requested dental consultation, but was told that there was no access to emergency dental care at Duane Waters Hospital. On January 27 he was seen by the dietician who did not appear to understand his need for pureed diet, and did not order him a pureed diet. Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 31d Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 20 of 60 September 8, 2005 Page #19 On January 28 Patient #1 complained that additional lesions were appearing despite the intravenous therapy. A physician, without examining Patient #1, ordered oral acyclovir 400 mg tid for thirty days, an inappropriate therapy for herpes zoster. On February 1511'1, five weeks after he arrived at DWH he was seen again by Dr. Howse, who did not examine him, or review his medications. On February 23, 2005 he reported that he was again having a recurrence of herpes zoster. The nursing staff did not call the doctor, but chose to "refer to MSP via physician board." COMMENT: Patient #1 has AIDS, severe sicca syndrome, which results in severe dryness of his mouth and esophagus, chronic hepatitis, and cirrhosis. He also had some degree of pancreatitis, which was not appropriately monitored. He received Inappropriate HIV medications for approximately 18 months, during which time he constanUy complained of abdominal pain. On September 30, 2002, the FDA issued a warning regarding the co-administration of Videx (001) and Tenefovir. It has been recommended since that time that Videx doses be decreased to 250 mg If the drugs are given together, and that in patients weighing less than 60 kg (132 pounds) the Videx dose be further reduced to 200 mg. Complications of these combination at the Videx 400 mg dose include decreased anti-viral efficacy, as well as pancreatitis and lactic acidosis. Except for one contrast X-ray, done in October, 2004, he had no diagnostic evaluation until I notified senior MDOC and CMS staff about his care. For over a year he complained of abdominal pain and had no endoscopy, no ultrasound studies, no CT scans, and no gastroenterology consultation. He told me that he would complain about abdominal pain while housed in Segregation and his complaints would be ignored by the security and medical staff. The pharmacy computer system at DWH failed to identify a well described Class 0 drug/drug interaction, and this inappropriate prescribing may have been responsible for Patient #1's persistent weight loss, and abdominal pain. Case 4:92-cv-00110-RAE Document 1897 Filed 09/12/2005 3111 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 21 of 60 September 8, 2005 Page #20 Although he was trying very hard to live, and to treat his complex medical problems, when he was finally transferred to DWH he was treated by the nursing and medical staff as someone who was about to die, and did not receive attention to his preSSing medical problems. When he developed Herpes Zoster, an extremely painful rash, the doctor failed to come to see him for four days. It was routine in Duane Waters Hospital for nurses to request physicians to examine patients and for physicians not to come. I have never before heard of physicians failing to respond to a nursing request to evaluate a patient, but according to the medical records I reviewed, and according to the Nursing Staff at DWH, this is routine. Patients in chronic status are at DWH to die, and they are seen on a monthly basis. As noted in the case of Patient #5 (described below), multiple acute painful conditions were ignored because he was classified, at the time of his admission to OWH, as a "chronic patient.Patient #2 Patient #2 was admitted to RGC on March 4, 2004. He was 29 years old. He weighed 180 pounds. He was known to have HIV infection. Fifteen days after admission, on March 19,2004, he had his physical examination. According the MSP note, "He refused rectal examination." Laboratory studies were drawn on March 22, 2004. They were not reviewed by the medical staff until April 15, 2004, twenty four days later. Repeat studies confirmed severe iron deficiency anemia, with a hemoglobin of 9.0. He was confirmed HIV positive and had 29 Tcells. Two of three tests for occult blood were positive. An 10 consultation was requested on April 15. The request was for two weeks, because of the anemia and low T-cells. The 10 appointment was given for May 26, 2004, six weeks later. On April 27 he was evaluated by an MSP who examined him and found "prolapsed hemorrhoids," and wrote, "would consider surgical referral for hemorrhoidectomy." On May 3, Patient #2 was evaluated for his RGC clearance, and told the PA that he had noticed blood on the toilet paper. On examination the PA did not see any hemorrhoids, but instead noted ulcerated anal warts. He Case 4:92-cv-00110-RAE Document 1897 Filed 09/12/2005 3IG Report of the Associate Monitor Revised and Redacted Hadlx v. Johnson Robert L. Cohen. MD Page 22 of 60 September 8, 2005 Page #21 was appropriately concerned that the patient had rectal carcinoma, since this is related to condyloma, and more common in men with HIV infection and low Tcells. The PA was concerned that the patient received timely Infectious Disease as well as gastroenterological consultation. The PA called Uz at eMS, arranged for 10 consultation on May 6, 2005, and put in a consult for gastroenterology. The next day The PA heard that the next available GI dinic was not until May 24, 2004. This was too long, so the PA called Dr. Hussein, the gastroenterologist, and arranged to have the patient seen the next week, on May 10. On May 111t1 patient was seen by Dr. Cohn of the 10 service. Patient #2 had Hepatitis C and HIV infection. Patient #2 was reluctant to start anti-viral medications. Dr. Cohn noted that the perianal lesion was bleeding and painful. Dr. Cohn was concerned that the lesion was an anal carcinoma, and agreed with the plan to schedule an exclslonal biopsy. He also felt that the patient would benefit from sitz baths, stool softeners, and suggested "that he should have some accommodation for having this chronic bleeding mass in his perianal area - whether that be a more accessible bunk, a cell that doesn't require ascending stairs, etc., but this is up to the discretion of the MSP." Two weeks later, on May 24, Patient #2 was seen by Dr. lIyas Hussain, the gastroenterologist. Dr. Hussain did not examine Patient #2 rectum. He recommended that Patient #2 have a colonoscopy, "for further evaluation." He wrote out this consultation on the 409 form, which was returned to SMT. A consultation request for the colonoscopy was faxed to CMS, but was pended by CMS while they waited for Dr. Hussain's dictation! The colonoscopy was finally scheduled for July 12, 2004. By the beginning of July, 2004, Patient #2 was in great pain, and he was having large amounts of malodorous drainage from the peri-anal lesion. On July 8, Deb Lange, the Nurse Practitioner at SMT, placed an urgent surgical consult to have Dr. Wisniewsky, a general surgeon, biopsy the lesion. The CMS scheduler, Unda KJeinhardt, told Deb Lange not to send a picture of the affected area. Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 Page 23 of 60 3111 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD September 8, 2005 Page #22· On July 12, 2004, three months after Dr. Hussain's was initially consulted to evaluate the patient, Patient #2 was brought into the endoscopy suite for his colonoscopy. Dr. Hussain looked at the peri-anal lesion for the first time. He noted that it was 6 cm by 10 cm with irregular margins and with a bleeding surface. The lesion was tender. He declined to do the colonoscopy. He wrote the lesion was likely a condyloma or anal wart. He wrote: "His MSP can schedule a 409 and consultation with a surgeon." On July 16 Dr. Wisniewsky, a general surgeon, saw the patient and said he was not able to perform a biopsy. He referred him for Plastic Surgery at the University of Michigan. For the next two months Patient #2 was housed at SMT. According to the medical record, the anal lesion drained copious amounts of foul smelling fluids. Dr. Mathai, the current CMS Associate Medical Director worked in SMT at that time. She told me that the odor of the discharge was extremely foul, spreading throughout the prison. It was not until September 21, 2004, more than five months after clinical staff had strong suspicion that Patient #2 had anal cancer, that a diagnosis was finally made. Biopsy showed locally invasive advanced squamous cell carcinoma. Two weeks later, on October 4,2005, by request of Deb Lange, NP, and Patient #2 was finally admitted to Duane Waters Hospital, where he had a single room, and appropriate nursing care. Dr. Crane, from the Infectious Disease Service saw him at Duane Waters and ordered long acting morphine sulfate for his severe pain. He spent another month at Duane Waters before he finally had surgery at Foote Hospital. By that time the lesion was inoperable, having invaded the buttocks. Patient #2 had surgery at Foote Hospital on November 4, 2004. The surgery was a diverting colostomy, bringing the end of the uninvolved bowel outside the abdomen into a colostomy. At operation the large fungating tumor was infected, making surgery difficult. There was considerable rectal bleeding post-operatively. The patient developed a deep vein thrombosis and septic pulmonary emboli. These are life threatening complications, which fortunately. Case 4:92-cv-00110-RAE Document 1897 Filed 09/12/2005 3Rt Report of the Associate Monilor Revised and Redacted Hadlx v. Johnson Robert L. Cohen. MD Page 24 of 60 September 8, 2005 page #23 Patient #2 survived. To prevent further emboli, an inferior vena caval filter was placed. After six weeks of hospitalization Patient #2 was discharged back to Duane Waters Hospital. He was begun on radiation therapy for his cancer, and after two weeks discharged back to SMT. Initial results from radiation therapy were encouraging with tumor shrinkage noted. COMMENT: When a 29 year old man with HIV infection presents with what appears to be an anal carcinoma, it is imperative that prompt diagnosis be made, and treatment initiated. In this case, whose outcome is not yet known, over five months passed before a simple diagnostic procedure was performed, another six weeks passed before the diverting colostomy was performed, and another six weeks past before definitive radiation therapy could be initiated. It Is possible that if in April he had been referred directly to a colorectal surgeon, a reasonable and usual approach to a patient with a rectal lesion, including anal condylomas, that his prognosis would have been significantly better. Patient #3 I interviewed Patient #3 on April 14, 2005 in the Segregation Unit in JMF. The first notes on the chart provided me were written at DWH by Mary Fowler. a speech therapist, who was trying to help Patient #3 communicate. She saw him on November 12 and on November 23, 2004. In her first note she advises the medical staff: For staff: Speaking strategies: 1. Stay calm, cool and collected. 2. Speak Slowly 3. Say the important words first; add more words slowly during conversation 4. Wait and listen to others Case 4:92-cv-00110-RAE Document 1897 Filed 09/12/2005 ~ Report of the Associate Monitor Revised and Redacted Hadbc v. Johnson Robert L. Cohen. MD Page 25 of 60 September a, 2005 Page #24 5. When frustrated or upset or dysfluent (stutters) take 5-10 deep breaths and relax. In her last note, on November 23, 2004, she noted that these strategies were working, and had improved his speech production and verbal expressiveness by 30%. According to the face sheet on his medical record, he was admitted to JMF from on January 10, 2005. He was first evaluated in JMF by Josia E. Smith, PA, on January 18, 2005. This evaluation was comprehensive, and included his enrollment in the Disability Chronic Care Clinic. He had suffered a severe stroke in September 2004, and had been hospitalized at DWH from 8/20/04 through 1/14/05, with two hospitalizations at Foote Hospital one for a new stroke which caused bleeding in his brain, and another for gastrointestinal bleeding Patient #3 was 51 years old. On admission to JMF he was noted to have chronic hepatitis (8 and C), hypertension and diabetes, with some kidney dysfunction. He had great difficulty communicating because of severe expressive aphasia, secondary to his stroke. At his January 18th visit Patient #3 did not complain of pain and was cooperative with the examination. He did not have any leg swelling, although he was noted to be very weak, and was noted to have significant lower extremity weakness, requiring a wheelchair. Mr. Smith referred Patient #3 to nephrology because of his renal disease, At the time of his stroke, on August 4,2004, Patient #3 BUN/Creatinine was 18/1.5. On January 4, 2005, just before he was transferred from DWH to JMF, his BUN and creatinine had risen substantially, and were now 50/2.5. His albumin had been chronically low, and was noted to be 1.9 on January 4, 2005. The required Nursing transfer receiving note was written on February 3, 2005, three weeks after Patient #3 was admitted to JMF. The note, written by Charles D. Boltjes, RN reaffirmed the medical classification (HCC-002) that Patient #3's medical needs could be met at any institution. Mr. Boltjes did not Case 4:92-cv-00110-RAE Document 1897 Filed 09/12/2005 Page 26 of 60 .' a"' Report of the Associate Monitor Revised and Redacted Hsdix v. Johnson Robert l. Cohen. MD September 8, 2005 Page#2S . make note of any of Patient #3's problems. He did not record any of his medications. He did not check his vitaJ signs. He described no physical deformities, and described his general appearance as good, although he did note that Patient #3 had "impaired communication" and was uncooperative and had been Interviewed in his cell, rather than the medical area. While at DWH, on December 1, 2004 Patient #3 had been referred to Nephrology because of his developing renal failure. The consultation, marked urgent, was faxed to CMS on December 2, 2005. CMS gave Patient #3 a telemedicine appOintment with Dr. Middlebrook on 8 AM, February 15, 2005 , two and a half months later. Patient #3 was not brought to his consultation on February 15, 2005. A nurse's note written at 1 PM on February 15 says" (No) Show, Per custody. AMA'd., CMS to reschedule." The next week, on February 22, Patient #3 complained of three days of painful swelling of his right arm. This had been not been noted before. Mr. Smith described the right harm as swollen, and hypersensitive. He described Patient #3 as being in pain, and noted that Patient #3 asked for vicodin. Patient #3 had been cautioned to avoid aspirin or NSAID's because of his recent gastrointestinal bleed. Mr. Smith noted that the laboratory studies he had ordered had not been done, and that the renal consult had not taken place, and re-ordered these. At Foote an ultrasound evaluation did not demonstrate any venous thrombosis as the cause of Patient #3's pain and swelling. He was sent back to the DWH ER where he was evaluated. He was given one 25mg dose of Ultram (Patient #3 weighed 232 pounds), X-rays of his right arm and shoulder were scheduled for the next morning (February 23,2005), and he was sent back to the segregation unit at JMF. The ER physician noted that Patient #3's MSP needed to develop a plan for long term management of Patient #3's severe pain. The next morning (February 23, 2005) Mr. Smith saw Patient #3 and told Dr. Faghihnia, about the patienfs problems. On February 24, 2005, Mr. Smith Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 Page 27 of 60 111 3 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. cahan. MD September 8, 2005 Page #26 again saw Patient #3, and noted that he had not been sent for his scheduled xrays. This encounter took place at the cell door. not in the examining room in the segregation unit. Mr. Smith ordered tramadol, 100 mg three times a day, for seven days, rescheduled the renal consultation for March 15, and scheduled a follow-up visit with Dr. Faghihnia in two weeks. The x-rays were taken on February 25.' On March 2, Dr. Faghihnia sent a test follow-up form to Patient #3, checking off the box "No clinically significant abnormality exists, therefore, no change in treatment plan is necessary.· If the xray was normal, then there was still no explanation for Patient #3's sudden onset of painful swelling of his right arm. A definite change in the treatment plan was necessary, in order to diagnose the cause of the swelling, and to assure that Patient #3 was free of pain. Mr. Smith's medication order was due to expire on March 3. It is difficult to imagine the thought or logic behind Dr. Faghihnia's decision to do nothing. On March 3, 2005, Patient #3 was again seen by PA Smith, who noted that his arm was still painfully swollen, and wondered whether there was a mass obstructing the venous flow from his arm. He discussed the case with Dr. Faghihnia, and ordered a CT exam of the chest, and referred a request for continuing the tramadol to Dr. Naylor. The consultation prepared by PA Smith requested an urgent CT scan, to be performed within two weeks of March 3. On March 5, Liz Klienhardt wrote an email to Lloyd Edwards, the CMS coordinator for JMF, notifying him that the CT had been pended. ON March 101h a nursing visit for the Disability Chronic Care Clinic took place. There is no evidence that the nurse spoke with Patient #3 , nor examined him. The note referred to PA Smith's "cell side evaluation." The note did not comment on Patient #3's pain, on the swelling of his arm, or on his ability to care for himself now that his right arm and both lower extremities were poorly functioning. Case 4:92-cv-00 11 O-RAE Document 1897 Filed 09/12/2005 3rd Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert l. Cohen. MD Page 28 of 60 September 8, 2005 Page #27 On March 141h, Dr. Faghihnia saw his patient, Patient #3 for the first time. He wrote: "Appears Alert, does not answer to questions properly and not cooperative. Speaks gibberish and feels like he has difficulty understanding the questions ... appears flustered and angry and speaks very fast, gibberish and loud. The spoken words are not complete and he does not finish any of his sentences. Sitting in wheelchair gets to scale with difficulty. HEENT: does not let me examine him well and does not take his hat off. Eyes. appears with round, equal pupils bilaterally, EOMr bilat. n Dr. Faghihnia did not order any pain medication, and scheduled a followup appointment in two weeks. He wrote in his note that a CT scan of the chest was pending. According to the chart, PA Smith had ordered the CT on March 3, but as of March 141h, it was pended by CMS. According to the medical record, the CT scan was never performed. On March 22, 2005, Patient #3 went back to Foote hospital for an ultrasound of his upper extremity which failed to show any vascular cause for the continued swelling. On that day he complained of pain to the nursing staff at 6 PM. He was sent to the Emergency Room. The DWH Emergency Room Staff noted that the edema had increased Significantly On March 24, PA Smith examined Patient #3 on his return from Foote Hospital, he noted that his arm was extremely painful to touch. He referred the patient to Dr. Faghihnia. On March 28, 2005 Dr. Faghihnia saw Patient #3. Again, according to Dr. Faghihnia, Patient #3 refused to allow any examination. He said that Patient #3 complained of pain all over, and that he was demonstrating drug seeking behavior. Dr. Faghihnia prescribed acetaminophen (Tylenol). On March 29, four and a half months after an urgent renal consult was requested from CMS, Patient #3 was finally seen by Dr. Middlebrook via telemedicine. Dr. Middlebrook's consultation was minimal. He did not review • Case 4:92-cv-0011 O-RAE Document 1897 Page 29 of 60 Filed 0911212005 3rc! Report of the Associate Monitor Revised and Redacted Hadbc v. Johnson Robert L. Cohen. MD September 8, 2005 page #28 any laboratory studies. He did not request to know the patient's blood pressure, he did not ask the patient any questions. He recommended an additional diuretic, and requested a follow-up visit in three weeks. On April 7, Patient #3 was not receiving any pain medication, despite his recurrent requests to the medical staff for relief of severe pain. No further effort was made to identify the cause of his painful arm swelling. Dr. Faghihnia did not place the consultation for the three week renal follow-up until April?, 2005. The consult was approved on April 12, 2005, and was scheduled for May 12,2005. This was five weeks after the initial conSUlt, two weeks beyond the three weeks requested by Dr. Middlebrook. On April 11, 2005 Drs. Naylor and Austin issued a memorandum entitled: JMF Segregation Chart Reviews. In their review of Patien #3's care they noted the following: "No show for a renal (clinic) on 212105. Abnormal lab (elevated TSH) not addressed in progress note. Action taken: The renal clinic was canceled that day. Patient was rescheduled for March 15, 2005. He did not go to his appointment on March 15, 2005. He indicated he did not feel well and was in pain. Has been seen by three MSP's all of whom are addressing the issue and increasing dosage. Patient will be referred for possible placement in C Unit... On April 20, 2005, Patient #3 was brought to Foote Hospital in extremis. He had never been transferred to C-Unit for infirmary care. The admission history and physical describes his having massive edema of his penis and scrotum, from which fluid was seeping, along with massive edema of both legs extending up to both of this thighs. He had abnormal laboratory tests showing acute renal failure as well as other electrolyte abnormalities. The day of his admission he developed respiratory failure and was intubated. On April 22, while Patient #3 was hospitalized, Dr. Faghihnia was asked by CMS to further delay the renal consultation until June 16, 2005. He agreed. I Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 3111 Report of the Associate Monitor Revised and Redacted Hadlx v. Johnson Robert l. Cohen. MD Page 30 of 60 September 8, 2005 page #29 Patient #3 died at Foote Hospital on May 9, 2005. I have been unable to review his hospital course because, according to Sharon Von Hom, Foote Hospital has refused to release his medical records because of HIPPA regulations. I have requested his hospital records on multiple occasions but have not yet received them. COMMENT: Patient #3 was obviously in tremendous pain when I saw him on April 13. He was refused necessary pain medication despite a gross and obviously painful physical abnormality, his massively swollen arm. His speech was severely limited by his dysarthria, which was caused by his stroke, b~t his physician, Dr. Faghihnia, refused to make the effort necessary to listen to his patient, and made no significant effort to relieve his intense pain. Patient #3 was housed In Segregation at JMF for two months before Dr. Faghlhnia, his physician, ever examined him. When he was finally seen, Dr. Faghihnia examined him in his cell, rather than in an equipped examination room. He was housed in segregation at JMF when he required intensive nursing care. The reason he was not transferred to C-Unit is not clear, but it may have been related to his Segregation status. This needs to be clarified, because patients in need of intensive nursing care cannot be denied access to that care because of their correctional status. If C-Unit cannot take people in segregation status, than Patient #3 should have been housed at DWH, as he had been before transfer to JMF Segregation. The administrative review performed by Drs. Austin and Naylor failed to make any minimal inquiry into Patient #3's obviously severely compromised state, and they made no effort to have him examined, to have the cause of his arm swelling identified, and to make sure that his pain was relieved. These administrative reviews are inadequate to the necessary task of assuring that patients locked in Segregation at JMF have appropriate access to medical care, the kind of access denied to Patient #3. If they had looked at Patient #3, they would have seen a very sick man, in need of urgent care. a Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 3n1 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 31 of 60 September B. 2005 Page #30 Patient #4 I interviewed Patient #4 on May 20. 2005. At that time he was housed in segregation. He is 33 years old, and has HIV infection. When he was admitted to RGC on January 6, 2005 he told the medical staff he had HIV infection, and complained of having frequent diarrhea. He was appropriately given an urgent evaluation and was seen and examined the next day by Dr. Gordon, who ordered the appropriate laboratory studies and his medications. Patient #4 had very low T-cells, 65, and a history of resistance to anti-viral medications. On January 13. and again on January 20,2005, Dr. Gordon noted that her initial physical examination had been lost. She repeated her examination on January 20. On January 21 she completed a referral for infectious disease consultation. The consultation was approved by CMS and scheduled for February 16. According to Patient #4, and confirmed by the medical record. he was placed in "Quarantine" in RGC because of an unresolved pending infraction from his previous MDOC imprisonment. He had been accused of sexual activity, and was placed in segregation. It is the policy of MOOC that HIV positive prisoners who are sexually active in prison are to be placed permanently in segregation. While in Quarantine at RGC. On February 16 he was called for his appointment to the Infectious Disease Clinic at DWH but was not allowed to go because of his segregation status. On February 18 Patient #4 was transferred from the Quarantine unit at RGC to the Segregation Unit at JMF. The patient was interviewed and examined at JMF on February 18 by an MD. On February 19. an RN spoke with the patient in his cell and scheduled him for an MSP visit on or about March 24.2005. On February 24 PA Smith examined Patient #4 as part of his Infectious Disease Chronic Care Clinic. He noted that he had missed his February 15 Infectious Disease Clinic appointment. and rescheduled it for March 2. He noted that his weight was 151, 8 pounds less than it had been on January 7, 5 weeks earlier. 1 Case 4:92-cv-00 11 O-RAE Document 1897 Filed 09/12/2005 3111 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 32 of 60 September 8, 2005 Page #31 PA Smith scheduled follow up MSP Chronic Care visits on March 21. May 16. and an RN chronic Care visit for August 31,2005. On March 2, security staff again failed to take Patient #4 to his Infectious Disease consultation at OWH. This was the second missed visit. On March 6 he sent in two kites. In one he requested to have his eyes check. An Optometry clinic was scheduled for March 7, but again, for the third time, Patient #4 was not taken to the dinic. The chart note from the Optometry clinic says that security staff said that the patient refused to come to the appointment. I asked him about this, and he told me that he had never refused any medical appointment. When Patient #4 sent a second kite on March 6 from his segregation cell requesting information about his missed appointment on March 2, the Nurse wrote back "You will be rescheduled." The patient was first seen by his assigned MSP. Dr. Faghihnia, on March 21. 2005. Patient #4 told Dr. Faghihnia that he had been having diarrhea for several weeks. and that the medication had made it worse. He recommended to the patient that he stop taking his anti-viral medications, but continue the Azithromycin and 8actrim. He scheduled a follow-up appOintment to see the patient in one month. and wrote "Patient is to be scheduled (with) Dr. CranellD ASAP. On March 30th the patient refused his scheduled Infectious Disease Clinic at DWH. On April 8.2005, Dr. Gordon became aware that Patient #4 had missed several 10 consultations and asked that he be called out. He was seen in his cell on April 19 when he again stated that he wanted to be seen by the Infectious Disease SpeCialiSt. On April 25. Dr. Faghihnia was scheduled to see the patient for the followup he had ordered on March 21. He did not see the patient. Instead he wrote MPatient dedined (refused) to be seen. Per officer report at seg unit." COMMENT: According to the Health Unit Manager at JMF. patients in the Segregation Unit are frequently denied transportation to DWH for specialty consultation. She told me that to counteract this practice. she had recently 6 Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 3111 Report of the Associate Monitor Revised and Redacted Hadlx v. Johnson Robert L Cohen. MD Page 33 of 60 September 8, 2005 page #32 established a procedure which required a nurse to interview every patient who "refused" to go to their specialty appointment. This is a good process. It must be initiated immediately, rather than retrospectively, at the time of "refusal: to assure that patients do not have their appointment cancelled. This patient was also refused access to Infectious Disease Specialty care while he was at RGC because he was in segregation status, referred to as "quarantine" at RGC. Patients in Segregation must be interviewed and examined in a confidential well equipped medical location. Special efforts, including immediate nursing intervention should be established to assure that these patients have access to specialty consultation, chronic care, and sick call. Patient #5 Patient #5 was admitted to RGC on April 6, 2004. He was examined by the medical staff on April 7th and 8th • He was diagnosed with AIDS, Chronic Hepatitis, asthma, and an ataxic gait which had left him wheelchair bound. He also had a severe dermatitis with excoriations noted all over his arms and legs. He said that he used benadryl every day to control the itching: Dr. Hutchison, the infectious disease consultant was notified that Patient #5 had been admitted. Appropriate laboratory studies were ordered, and he was referred for Infectious Disease Consultation. He was given an inhaler, an antihistamine, Azithromycin and bactrim, because he had not been receiving antiviral medications for several months, and there was concern that his T-cells were low, placing him at risk for pneumocystis pneumonia. T cell and viral load studies were available at the facility on April 15, revealing an extremely low T-cell count of 28, and a very high viral load. On April 12, he requested assistance with his wheelchair. It was noted that he had no wheelchair accommodation. In response, on April 28 he was evaluated by physical therapy who agreed with Patient #5 that he needed his wheelchair whenever he had to travel significant distances. He couid walk Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 Page 34 of 60 nt 3 Report of the Associate Monitor Revised and Redacted HarilX v. Johnson Robert L. Cohen. MD September 8, 2005 Page #33 around his cell and for short distances. An accommodation was given to him. Although Dr. Hutchison was notified on April 7,2004 that Patient #5 had been admitted, as of April 30, 2004 he had not been started on any anti-viral therapy. On April 30 he was begun on nortryptilline, to provide additional treatment for his peripheral neuropathy. On May 3. 2004, Dr. Faghihnia referred to Patient #5's condition as "endstage AIDS with painful neuropathy," yet ordered no specific analgesic medication for him, only continued his nortryptilline. On May 4, 2004, Patient #5 put in a kite asking for assistance with a raSh, and complained of pain in his legs and back. He was seen by a nurse on May 5, 2004 who diagnosed his skin problem as ·contact rash, (secondary to End Stage AIDS (042) and prescribed 1% hydrocortisone. There was no response to his leg or back pain. On May 7, he again requested medical care for "many numerous complaints." There was no response from the nursing or physician staff at RGC. A chart review conducted at JMF on May 18 noted that Infectious Disease and Psychiatric referrals were pending and said ·At this tim~ it appears his transfer is inappropriate to this facility. If anything he should at least be placed where hospital is very accessible. His intake screening at JMF was completed on May 20, and he was referred to Psychiatry. and to the eMS coordinator regarding his pending Infectious Disease consultation. He was given a referral to his MSP, Dr. Faghihnia, for May 25. On May 23, he submitted a kite with the complaint "CHRONIC LEG PAIN." A nursing evaluation performed on May 24 described his problem as •Altered comfort? HIV neuropathy." The nurse noted he was to see Dr. Crane of Infectious Diseases on May 26 at 8 AM. He was given no treatment for his pain. On May 25, Dr. Faghihnia examined Patient #5 and found no physical abnormalities except for an extensive maculo-papular rash and trace ankle edema. He was able to perform a Npartlal fundoscopy" only. Patient #5 told him that his legs swelled when he walked. Dr. Faghihnia recorded this information Case 4:92-cv-00110-RAE Document 1897 Filed 09/1212005 Page 35 of 60 , 3111 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert l. Cohen. MD September 8, 2005 Page #34 with an exclamation point. Dr. Faghihnia found no leg weakness and decided that Patient #5 had no need for a wheelchair. He cancelled the wheelchair, cancelled the neurontin, cancelled the ranitidine, cancelled his albuterol inhaler, and decreased the benadryl to 25 mg at night only. There is no explanation in the note as to why he was discontinuing these three medications and drastically decreasing the dose of the fourth. Patient #5 was receiving benadryl 50 mg three times a day for his chronic itching, neurontin for his HIV neuropathy, and ranitidine for gastroesophageal reflux. There is no indication in the note that Dr. Faghihnia informed Patient #5 that he was discontinuing these medications. Dr. Faghihnia asked that a punch biopsy of Patient #5's skin be scheduled. He did order a "Detail for walker x 6m." He was seen on May 26 by Dr. Crane who ordered Ziagen 300 mg bid, reyataz 300 mg qd, Norvir 100 mg qd, and Videx EC 400 mg. This medications were ordered six weeks after his T-cell count of 28 had been received by the facility. On June 9, Patient #5 requested refills of his benadryl and neurontin, but they were not available because Dr. Faghihnia had cancelled them. Dr. Faghihnia reviewed Patient #5's chart on June 29 and examined him. He noted that Patient #5 complained of severe numbness in his feet, and inability to feel his feet in the morning, as well as severe itching. Dr. Faghihnia examined his feet and documented that he had very poor sensation, which he attributed to peripheral neuropathy secondary to HIV infection. He reordered medications, now increasing Patient #5's benadryl back to 50mg three times a day, but did not provide any treatment for the peripheral neuropathy. On July 6 he wrote that Patient #5 "was stable and dOing well now," but there is no indication that he ever examined Patient #5. There are no subjective or objective elements recorded. Laboratory studies were ordered on July 13, 2004. These studies were initially reported back on July 15, but no review of labs took place until August 9. , Case 4:92-cv-00110-RAE Document 1897 Filed 09/1212005 Page 36 of 60 n1 3 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD September 8, 2005 page #35 Of note is the fact that these July 13 studies were the last laboratory studies of Patient #5's liver and renal function until he was hospitalized on December 1, 2004. On July 14th he was seen again by Dr. Crane who recommended that he be transferred to C Unit because he needed more nursing care than was available to him in general population at JMF. This transfer did not take place. On July 17, he complained of increased pain in his right hip. He was seen by a nurse who did not examine his back or leg, and prescribed acetaminophen (Tylenol). He was not referred to a physician. On July 21, 2004, he again complained of pain in his back and side. He was called to be seen by the Nursing staff on July 22 but went to the yard instead. On July 26, he submitted another kite, apologizing for missing his call out, and again complaining of pain on the right side of his body, especially his hip and leg. He also complained of diarrhea. He was seen on July 27 by a nurse. His blood pressure was 153/108. No examination of his leg or back was performed. He was given loperamide for his diarrhea. On July 27, he submitted a kite asking why his benadryl had been discontinued, and requested renewal of his hydrocortisone and petroleum jelly. He also asked for a pillow because of his hip and leg pain. The nurse wrote that she had given the kite to Or. Faghihnia, but that he was not going to renew the hydrocortisone cream or the petroleum jelly. Dr. Faghihnia did not examine the patient, but he did order the extra pillow On August 3, Patient #5 complained that he was still having problem with his right side. The nurse did not examine him, but told him he would be seen on August 19. On August 4, he submitted a kite complaining of right sided pain. He was seen the next day by a member of the nursing staff who noted that his blood pressure was 148/89, and referred his "chronic musculoskeletal complaints to the MSP for evaluation. Dr. Faghihnia examined him on August 9 found a completely normal physical examination of the leg and hip, and diagnosed Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 3rd Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 37 of 60 September 8, 2005 Page #36 sciatica. However, because of the patienfs chronic hepatitis, he told him not to take Tylenol or motnn. He prescribed nothing for the pain. On August 17, Patient #5 submitted a kite in which he again complained of pain in his right side. Dr. Faghihnia did not examine the patient, but he did recommend tennis shoes be provided to him because of his medical condition and because he was indigent. On August 25, Patient #5 submitted another kite, saying "right side still hurts." He was seen by a nurse on August 25 who recorded that he had pain in his right hip and thigh for one month, but that it was worse now. The nurse noted swelling of his right foot. He was seen the next evening, August 26, in the DWH ER. PA Smith evaluated him and found him to be in severe pain, unable to bear any weight. Any movement of the hip resulted in severe pain. PA Smith gave him 50 mg of DemerollM, and sent him to the Foote Hospital ER where he arrived early in the morning of August 27. His blood pressure at that time was 167/98. An x-ray of his hip was normal. The Foote Hospital emergency room physician diagnosed lumbar radiculopathy. He was given an injection of Toradol 30mg, and 10 mg offlexeril, and sent back to the DWH ER. PA Smith received him back the DWH ER and referred him to Dr. Faghihnia for follow-up. Dr. Faghihnia did not see the patient. HIV specific laboratory studies were obtained on August 30, 2004. They were received at JMF on September 1, 2004. Dr. Faghihnia did not see review these studies until October 15, 2004. He was seen by Dr. Crane for Infectious Disease Consultation on September 1, 2004. He was responding very well to the ant;'viral therapy. Patient #5's CD4 count had Increased from 28 to 184 in two month's time, and his viral load had decreased dramatically. Dr. Crane felt that the hip pain was probably not aseptic necrosis, since the x-ray was normal. He recommended further radiologic evaluation if the pain continued. Dr. Crane noted that the right leg was significantly more swollen than the left. He said that this could be Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 Page 38 of 60 R1 3 Report of the Associate Monitor Revised and Redacted Had/x v. Johnson Robert L. Cohen. MD September 8, 2005 Page #37 attributed to venous insufficiency. He dictated his note on September 1 and It was transcribed on September 2. The handwritten note was returned with the medical reoord on September 1. Dr. Faghihnia saw both the handwritten note and the dictation on September 9. His pain continued. On September 1-2,2004 he was seen in the DWH ER and given toradol intramuscularly for severe pain of his right hip and leg. In the emergency room swelling of both legs were noted, the right more swollen than the left. He was discharged back to see his physician, Dr. Faghihnia. Dr. Faghihnia did not see the patient. On September 10 he requested sick call and was again seen by a nurse for his continuing complaint of constant right lower extremity pain, hip pain, and swelling of his leg. His blood pressure was again elevated, For the first time he was prescribed three days of tramadoI 50 mg, three times a day, with follow-up scheduled for September 13 With PA Smith. PA Smith took away Patient #5's wheelchair, and did not re-order any pain medication. On September 15, Dr. Faghlhnia reviewed the chart. He did not examine the patient. On September 17, Patient #5 was seen for his continuing pain. No medication was given to him. PA Smith was notified. The patient was encouraged to elevate his legs. On September 20, he again requested medical care for pain in his feet and legs. He was seen two days later, on September 22, and prescribed ibuprofen 200 mg every 4 to 6 hours. No referral to his MSP was made. On October 4 Patient #5 requested medical assistance for right sided lower extremity pain. He also asked for a refill of his benadryl. He was not seen for three days, until October 7. At that time he was evaluated by a nurse who diagnosed venous insufficiency as the cause of his pain, and ordered 200 mg of ibuprofen. The nurse referred the patient's complaint of pain to Dr. Faghihnia for consideration of additional pain medication. Case 4:92-cv-00110-RAE Document 1897 Filed 09/1212005 3n1 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 39 of 60 September 8, 2005 Page #38 On October 8, Dr. Faghihnia wrote a note in the chart. He did not examine the patient. He did not ask the patient any questions. He did not consider the request by the Nurse from October for evaluation of the patient's need for additional pain medication. He wrote that the patient's condition was stable. He also noted that there was no need to have him seen any sooner by the infectious disease consultant. Dr. Faghihnia note says "He is informed." On October 10 Patient #5 had an emergency nursing evaluation for his complaint of severe back and hip pain. The nurse referred him to DWH ER. On examination at DWH his pulse was noted to be 123/minute, approximately twice normal. No evaluation of the cause for this abnormality was pursued. The physician at DWH diagnosed the patient as having a deep pain thrombosis (blood dot) in his right leg, and gave him an injection to prevent clotting, recommending that a doppler study of the veins of the lower legs be performed the next morning. The DWH ER physician called Dr. Faghihnia and told him of his recommendation. He was seen five days later by Dr. Faghihnia at his chronic care clinic. His pulse was 123/minute, approximately twice normal. He had lost 10 pounds in the preceding month. He complained of severe pain and swelling in his legs which he said made walking difficult. Dr. Faghihnia noted that he had bilateral swelling of his legs, much greater on the right than the left. Dr. Faghihnia wrote: He is not walking toady and comes to the clinic with a wheelchair that he has borrowed from a friend. He states that (he) has a lot of pain in his legs and feet and is unable to walk due to severe pain. He transfers to the scale and exam table very slowly. He has lots of medical problems and lots of pain due to his HIV neuropathy probably. He however does not have any problem to become whee/chair dependent and his prognosis would be much worse if he does not try to keep moving and the dependent edema in legs would be exacerbates (sic). He is Case 4:92-cv-00110-RAE Document 1897 Filed 0911212005 3'" Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert l. Cohen, MD Page 40 of 60 September 8, 2005 Page #39 explained a lot about all these and he finally accepts to be cooperative and would try to be more active. Neurontin is a minimally effective medication for pain. It had not significantly helped Patient #5 in the past. He failed to provide any medication which would provide adequate pain relief. He did not schedule a follow· up appointment within the next few days or week to determine if the medication he did prescribed was effective in relieving the severe pain Patient #5 was experiencing. Dr. Faghihnia made no effort to determine the cause of Patient #5 pain. He wrote in his note that a Doppler study longing for DVT was normal. In fact, the study was not performed until one week later, on October 22,and was not normal. The study was unable to visualize the peroneal vein. This study did not rule out a deep vein thrombosis. Of note is that on October 15, in addition to his visit with Dr. Faghihnia, Patient #5 was told by the nursing staff that he incurred a co-payment charge when he sought medical care. Patient #5 saw Dr. Crane, the Infectious Disease Specialist on October 3, 2004. Dr. Crane noted that Patient #5 had ~constant exquisite sharp pains in the H right hip area with increased swelling of the right leg. Dr. Crane was concerned about the severity of the pain, believed that Patient #5 had avascular necrosis of the hip, and referred Patient #5 to the DWH ER to arrange for urgent admission to the Orthopedic service at Foote Hospital in order to obtain an MRI or CT scan of the hip. Patient #5 was sent to the Foote Hospital ER. An emergency CT scan was performed and again showed a normal hip. Patient #5 was returned to DWH and subsequently to JMF the next day. His pain and leg swelling continued unabated, and no further workup was planned to identify the cause of his constant distress. Dr. Faghihnia initialed the November 3, 2005 ER visit note from Dr. Howze at the DWH ER on November 21, 2005 almost three weeks later. He never saw the November 4, 2005 ER note from DWH indicating that the CT exam of the hip was normal -there was no fracture, no arthritis, no avascular necrosis. He never saw Patient #5 again. Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 3111 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 41 of 60 September S, 2005 Page #40 On December 4, 2004, Patient #5 was again sent to the Foote Emergency Room for painful leg swelling and abdominal pain. Routine laboratory studies revealed that his kidneys were not functioning, and an emergency CT scan showed that his pelvis was filled with tumor, which was blocking his kidneys. His BUN was 104 and his creatinine was 7.3. An emergency CT scan of the abdomen and pelvis on December 4, 2004 showed bilateral obstructed enlarged kidneys, with multiple masses blocking the flow of urine. These masses were Non-Hodgkin's Lymphoma, a common tumor found strongly associated with AIDS. Patient #5 was hospitalized on December 4, 2004, seven months after he first complained of leg pain and swelling on May 4. Patient #5 had surgery involving the placement of stents to allow urine to flow out of his kidneys, and to biopsy the mass and diagnose his lymphoma. On December 8, 2004. at 11 :12 AM, Patient #5 was discharged back to Duane Waters Hospital for comfort care. According to Dr. Siddiqi's discharge note, Dr. Axelrod, the oncologist felt that because his prognosis was poor, he should not receive chemotherapy, but should be transferred back to Duane Waters for comfort care. Two hours later, Dr. Siddiqi dictated an addendum, canceling the discharge, and noting that Dr. Axelson had decided to treat the patient with chemotherapy. He was diagnosed with bilateral deep venous thrombosis as Foote Hospital and treated with anti-coagulation therapy. On January 17, 2005, Patient #5 was discharged back to Duane Waters Hospital. In his discharge note, Dr. John Axelson wrote: Obviously for someone who has been hospitalized this long, it takes a specific review of the chart, but I would like to try and summarize in as much detail as possible in view of the fact that he is being transferred back to Duane Waters Hospital. .... The case management has kindly left a note that his current length of stay of 44 days at this point has run up charges of at least $170,000. She is Case 4:92-cv-OO 11 O-RAE Document 1897 Filed 09/1212005 ani Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 42 of 60 September 8, 2005 Page #41 recommending transfer back to Duane Waters and is concerned that eMS may no longer justify ongoing inpatient care. He was discharged back to Foote Hospital on January 17th • Foote Hospital recommended that he be continued on anti-coagulation therapy, that he be continued on Zyvox for Vancomycin Resistant Enterococcal Infection, and that he be given Total Parenteral Nutrition (TPN) to improve his nutritional status so that when he returned to Foote Hospital in a week he would be better nourished, and more able to tolerate chemotherapy . .He was readmitted to Duane Waters Hospital. Anticoagulation therapy for his deep vein thrombosis was not ordered. TPN was not ordered. Morphine as MS-contin was ordered for pain. After his initial admission evaluation to the Duane Waters Hospital on the morning of January 17, 2005, he was not seen again by a physician or MSP, despite the fact that he was in constant pain. He was transferred back to Foote Hospital on January 24, 2005, for his next round of chemotherapy. At Foote Hospital, Dr. Madani's January 24 admission note says: II . . • he was discharged about a week ago .... And .. recommendations to do anticoagulation with Lovenox and then recommendation to do TPN for his poor nutritional status. As I said, he is not receiving any TPN at Duane Waters Hospital and he is not receiving any Lovenox, but he has been receiving Zyvox twice a day as prescribed. ... ... The patient told me that he has had a very bad week. He has .. .been having increasing abdominal pain. He has been having increased constipation and he has been having increasing nausea and he vomited twice yesterday evening and today this evening. n Additional attempts at cancer therapy were attempted at Foote, but were unsuccessful. He was discharged back to Duane Waters Hospital on February 4. He was readmitted to Foote for one day on February 10, than discharged. Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 sri! Report of the Associate Monitor Revised and Redacted Hadlx v. Johnson Robert L. Cohen. MD Page 43 of 60 September 8, 2005 Page #42 Patient #5 was readmitted to Duane Waters Hospital on February 10 discharged, and readmitted, and died two weeks later on February 19, 2005. COMMENT: This is a very tragic case. It demonstrates several recurrent deficiencies. A patient with AIDS with severe pain in his hip with significant swelling on the side of the pain went for seven months without treatment of pain or a diagnosis of his treatable cancer. Diagnostic efforts were minimal, complaints of pain were ignored or trivialized. When a diagnostic test was indeterminate, or ruled out a suspected diagnosis, the response was to assume the patient was exaggerating his pain, and further diagnostic tests were not scheduled. Patient #5 suffered tremendous pain for seven months and received no treatment for it. His lymphoma was present for months, causing an obvious physical sign of painful unilateral swelling of his right leg. Instead of aggressively seeking a diagnosis, his physician dismissed his complaints, viewing him as a prisoner seeking pain medication, rather than a patient seeking help. When the Doppler study was indeterminate, Dr. Faghihnia did nothing. When the CT scan of the hip was negative, Dr. Faghihnia did nothing. The fact that Patient #5 did not have avascular necrosis of the hip did not explain why his right leg was swollen and painful, but it was sufficient for his physician to stop looking for other causes of his pain. Non-Hodgkin's lymphoma (NHL) in HIV infection is a serious condition, but is often extremely responsive to chemotherapy. The oncologists at Foote told Patient #5 that he had only a three month prognosis for is illness, which is not consistent with the literature. (M C Robolinand others. Clinical features and predictors of survival of AIDS-related non-Hodgkin's lymphoma in a population-based case series in Sydney, Australia. HIV Medicine 5(5): 3n-384. September 2004.: R Biggar and others. Survival after cancer Diagnosis in Persons with AIDS. Journal of Acquired Immune Deficiency Syndromes 39(3): 293-299. July 1, 2005; J Acquir Immune Defic Syndr 2002: 30:478-484}.} The Foote hospital oncologists recommended that he not receive any treatment. Mean disease free interval survivals for NHL patients with HIV infection on anti-viral Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 Page 44 of 60 ~. 111 3 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD September 8, 2005 Page #43 therapy are doser to two years than three months. Had he been treated aggressively with appropriate chemotherapy five or six or seven months earlier, before he developed acute renal failure, his response would probably have been much better. Additionally, the first week Patient #5 spent at DWH following his discharge from Foote Hospital revealed the general practice at DWH during this period. Although Patient #5 was acutely ill, suffering from the complications of chemotherapy, decubitus ulcers, and severe pain (9.5/10 when he was asked by the nurses), he was admitted to the hospital as a "chronic patient." This meant that the medical staff were required to see him once a month. In this case, after his admission, he was ~ seen again by an MSP. On several occasions Dr. Howse was called by the Nursing staff about Patient #5, but she never came to see him, and actually reduced his pain medication via a verbal order. During 2004, and through April of 2005, this was routine practice at Duane Waters Hospital. Patient #6 Palient #6 bled to death from an ulcer. He had a history of colon cancer. Two years before. on October 26, 2003, while at RGC, complained of abdominal pain, and of throwing up coffee grounds. He was diagnosed at that time with a bleeding duodenal ulcer. On the problem list on the front of his chart there is an entry; "PUD = GI Bleed. 10/30/03." In 2004 he was diagnosed with colon cancer and had a partial colostomy. Patient #6 complained of epigastric (abdominal) pain on 1/21105. His Temperature was 93.7. He was given ranitldine (zantac) and sent back to his cell. No blood test was ordered. No stool guaic test was obtained (although one was ordered). The PA who saw Patient #6 wrote: "Pt refused any further testin~, agreed to do hemocult Will start a trial of zantac and Tylenol for pain. Advised Case 4:92-cv-00110-RAE Document 1897 Filed 09/12/2005 31d Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen, MD Page 45 of 60 September 8, 2005 Page #44 to kite if not improved." Forty eight hours later Patient #6 bled to death in his cell from an acute bleeding duodenal ulcer. COMMENT: It is possible to diagnosis the presence of gastrointestinal bleeding in seconds with a stool guaiac test (test for blood in the stOOl). When a patient with a history of colon cancer and a bleeding duodenal ulcer complains of acute abdominal pain, a digital rectal examination along with a test for blood in the stool is mandatory. No rectal examination was performed. No stool guaiac test was done. According to the chart note, Patient #6 did refuse testing at the time of his encounter, but the MSP should have explained to him the importance and simplicity of the required testing. Patient #6 had not complained of abdominal pain for more than one year. He was suffering an acute abdominal process, and he was treated for a stomach ache. Had the minimal necessary care been provided him, he would have been diagnosed immediately, and probably treated successfully. Patient #7 Patient #7 was 52 years old when he died on June 6, 2005 of metastatic lung cancer. Lung cancer is a devastating and common disease. and, unless detected early, it rapidly spreads and has a fatal outcome. Patient #7 first requested medical attention on April 4. 2005. He sent a medical kite complaining of a "lump on collar bone." He complained of weight loss, malaise, and chills. He was seen by Charles Boltjes, an RN at JMF the next day, April 5, and immediately referred to Josiah Smith, PA, who confirmed the present of I(eft) supraclavicular (above the clavicle) .. tender firm, fixed nodes." He suspected some kind of cancer, either gastrointestinal, lung. or lymphoma. He ordered immediate laboratory studies and a chest x-ray. The next day laboratory tests showed a dangerously elevated potassium level, PA Smith was informed of the results and sent the patient to the DWH ER Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 Page 46 of 60 111 3 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD September 8, 2005 Page #45 for management. At DWH a repeat potassium level and an EKG were normal, and Patient #7 was sent back to JMF. Mr. Smith scheduled a follow-up appointment on April 8. On April 8 Mr. Smith wrote that the chest-x ray was "not available yet. Will flu CXR on Monday. Monday, 4/11 will request urgent bx (biopsy) of L subclavian lymph nodes.· On April 11, Mr. Smith was told that the x-ray, which had been taken on April 5, showed a right peri-hilar mass. He wrote: "Will generated urgent cr Chest with IV contrast and urgent L Supraclavicular lymph node Bx. Discussed with Dr. Faghihnia." Mr. Smith scheduled a follow appt with himself to review the results of the CT scan and Biopsy. Dr. Faghlhnla did not see the patient. Two weeks later, on April 25, 2005. no CT scan had been obtained. and no Biopsy had taken place. No surgery appointment had been scheduled. Dr. Faghihnia did not see the patient. PA Smith re-submitted the emergency consultations he had submitted two weeks before. Mr. Smith next saw Patient #7 on May 4, 2005, nine days later. At that time he complained that for the past week he had nausea and vomiting, increased cough, he felt poorly, and had night sweats and chills. He noted that the CT scan, performed on April 26 showed a right lung mass. The CT scan was read on April 27 at Foote Hospital. The report describes a large irregular mass extending from the bronchus intermedius into the right middle and lower lobes of the lung. The Foote Hospital radiologist did not contact any clinician at JMF about the results of the study. On May 4, 2005. while he was evaluating Patient #7, PA Smith obtained a fax of the study from Foote Hospital. Also, on May 4, PA smith obtained the results of the biopsy performed on April 28 by Dr. Wisnewski. Dr. James C. Niewenhuis, a pathologist, read the biopsy and notified Dr. Wisnewski by telephone at 2:00 PM on May 2, 2005, that the lymph node showed metastatic adenocarcinoma. Dr. WIsnewski did not notify the patient. Dr. Faghihnia, or Mr. Smith of the results of the Biopsy. On May 4, PA Smith spoke with Or. Trimble at Foote Hospital and arranged for the patient to be admitted to the hospital for treatment of his cancer. • Case 4:92-cv-00110-RAE Document 1897 Filed 09/1212005 3111 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 47 of 60 September 8, 2005 Page #46 Evaluation by the oncologists at Foote Hospital revealed that the cancer already involved the brain and the liver. A plan for radiation therapy and chemotherapy was developed. On Friday evening. May 6. 2005, at 2110 (11 :10 PM) Patient #7 was retumed from Foote Hospital. There is a very brief note ER note in the chart. The patient was sent back to JMF. He was not seen at JMF by Dr. Faghihnia, his physician. He was seen on May 9, at 4:46 PM by PA Smith. Mr. Smith referred him to see Dr. Faghihnia. He was seen for the first time by Dr. Faghihnia on May 23. seven weeks after he first presented with weight loss, cough. and lymphadenopathy. Dr. Faghihnia did not see him again. On Saturday morning, June 4, at 6:39 am. Patient #7 complained that he had been unable to eat for three days and that he had pain in his lower back and abdomen. His blood pressure was 88/70 and his pulse was 130. He was taken to the DWH ER and admitted there, were he died early on the morning of June 6, 2005. COMMENT: Mr. Smith ordered a STAT chest X-rayon April 5, but he did not receive the report of the grossly abnormal study until April 11, even though he sought to obtain the report three days earlier, on April 8. CMS has said that abnormal radiologic studies will be reported immediately, but that did not happen. Although on April 11 Mr. Smith. Mr. Smith requested an urgent CT of the Chest and an urgent lymph node Biopsy within one week. describing in detail Patient #7's condition and the need for rapid diagnosis, by two weeks later, CMS had not done anything. When the CT of the chest was read and showed a probably extensive malignancy. the radiologist did not notify Patient #7 or his physicians of his finding. Dr. Wisnewski was called with the result of the pathology. but failed to notify Patient #7, or his physicians. Dr. Faghihnia was told by Mr. Smith on April 11 that his patient. Patient #7, had a mass on his chest x-ray. Dr. Faghihnia did not make any effort to assure that his patient received timely diagnostic evaluation. He did not speak with the oncologists at Foote Hospital to find out what kind of therapy they were Case 4:92-cv-00110-RAE Document 1897 Filed 09/12/2005 aid Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L Cohen. MD Page 48 of 60 September 8, 2005 Page #47 proposing, and he did not speak with Patient #7 until May 23, 2005. According to that note, he did not schedule any follow-up appointment with Patient #7 to make sure that he was receiving necessary palliative care along with his chemotherapy and radiation. Mr. Smith is to be commended for his repeated efforts to provide care for Patient #7. His efforts were frustrated by the repeated failure of radiologists to report significant gross abnormalities, the failure to obtain urgent studies in a timely manner, and the surgeon's failure to report the results of his biopsy to his patient, or to his patient's physician. His diagnosis was unnecessarily and repeatedly delayed for one month. During the last month of his life, while he was receiving intensive chemotherapy and radiation therapy, his physician, Dr. Faghihnia, failed to monitor his care, saw him only once, and failed to admit him to DWH in a timely manner. Patient #7 was receiving chemotherapy and radiation therapy for metastatic lung cancer which had spread to his brain and to his liver. He was extremely weak. When he was finally admitted to DWH he was in pain. He should have been housed in a supportive nursing environment during the last month of his life. Patient #8 Patient #8 was admitted directly to the Segregation Unit at JMF on June 15, 2005. He had been aooW" (Out on writ) since September 2, 2004, According to Jeffrey Schulcz, RN, no chart was available when he saw the patient on June 15. The patient told him that he was being treated for a an MRSA (Methicillin Resistant Staphylococcus Aureus) infection of his leg. Mr. Schulcz did not examine the patient. He did not obtain vital signs. His note reads: "Comments regarding objective findings: Pt has red Biohazard bag wrapped around L lower feg. Under Blo bag has muftipie layers of ABO pads and gauze. Unable to examine thoroughly as pt in dress in case in seg. Pt pulled dressing down from knee, L lower feg red and extremely swollen. Pt states that Case 4:92-cv-00110-RAE Document 1897 Filed 09/12/2005 31d Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L Cohen. MD Page 49 of 60 September B, 2005 Page #48 skin on back of leg sloughs off when touched and that lower leg constantly weeps clear to yel/ow fluid." Patient #8 was sent to the DWH ER. Nurse Schulcz wrote: "Unable to care for pt needs at JMF. Sent to DLW (DWH?) for eval and admission. Will flu with clinic MSP on discharge." (Mr. Schulcz's note is timed at 7:33 PM on the SERAPIS system. He arrived at DWH at 6:00 PM. There is no functional SERAPIS terminal in the Segregation Unit, and the note was probably entered later). At the Dwayne Waters Hospital ER Patient #8's medical history was obtained. He had a history of a heart attack, had received 3 coronary artery bypass grafts in 2000, and was being treated for diabetes, hyperlipidemia, hypertension, and gout. His medications included: Nitroglycerin, Lopressor, vasotec, lasix, potaSSium, norvasc, lovastatin, glipizide, allopurinol, zyvox (for methicillin resistant staph - MRSA) as well as multiple pulmonary inhalers. His leg was chronically infected, but for the previous several weeks it had become very swollen, painful and clearly infected. Dr. Pacelle, the physician in the DWH ER sent Patient #8 to Foot Hospital for evaluation and treatment. He arrived at the Foote Hospital Emergency Room at 2116 on June 15. He was examined and laboratory studies were obtained. Patient #8 was noted to be in severe pain. He said that he had been receiving antibiotics for MRSA for the past two days. He said that he had been hospitalized and had received a transfusion for anemia, but that he was discharged from the hospital at Clare because he didn't have any money. Laboratory studies at Foote were extremely abnormal. Patient #8 was severely anemic. His hemoglobin was 8.4, slightly more than half normal, despite a recent blood transfusion. Foote Hospital records from 2001 showed that his hemoglobin at that time had been 11.9. His sodium was significant decreased at 129. He had blood in his stool. Dr. Farhat, the physician at Foote, wrote a comprehensive, and distressing discharge note. He stated that "Dr. Pacelle, sent him here to rule out a deep venous thrombosis and a possible Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 Page 50 of 60 II " 111 3 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert b. Cohen. MD September 8. 2005 Page #49 admission for cellulites. Dr. Pacelle said that they did not .have any beds there for the patient.· Dr. Farhat. in the section of the discharge note headed "MEDICAL DECISION MAKING" wrote: "/ discussed the case with Dr. Qureshi, who is in the PAC-group (critical care physician practice at Foote), to see if he would like to admit him to transfusion with a workup his anemia and occult hematochezia (blood In the stool). Dr. Qureshi, after discussing this in depth with me, did not feel that is was emergent to admit the patient and that he could be worked-up as an outpatient at Duane Waters Hospital. He said that he ought to give him one unit of packed red blood cells reason being that he was a congestive heart failure, which we will give that over three hours. We will send him back. He will need to follow-up in the gastrointestinal clinic there. Also Dr. Qureshi said that the patient would not benefit from admission for antibiotics because he is currently on the Zyvox. He has only been on it a couple of days and he needs to be on it longer. I then relayed this information back to Dr. Pacelle at the prison. I told Dr. Pacelle to repeat the cac tomon'Ow(.) if it is worse. (t)he patient is to come back. The patient will need to get into the gastrointestinal clinic as soon as possible for workup of his anemia and hematochezia. They could do an anemia workup there at the prison. The patient is to come back here if has black stool, blood in the stool, worsening or other problems or concems. He is to continue his Zyvox. I also told Dr. Pacelle that he needed to get an Infectious disease consult. All this workup I believe can be done at the prison, as Dr. Qureshi felt was appropriate. Dr. Qureshi did not feel that he needed to be admitted." These instructions were written on the Foote Hospital"lnstructions for Follow-up Care" which accompanied the patient back to the DWH ER. " Q Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 3n1 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 51 of 60 September 8, 2005 Paae#5Q Patient #8 arrived back at DWH at 5:30 in the morning of June 16. A esc was drawn, and he was sent back to JMF. At 1130 he was seen by a physician in the Segregation Unit. The physician (Dr. Gordon?) said that she did not have access to the medical record. Her examination was limited to Patient #8's left leg. She did note that "Patient #8 also reports melanotic stools X 3 weeks - he denies being on iron supplements - Again without his chart this is not verifiable: She noted that he had received coronary artery bypass grafts in the past. Dr. Gordon did not examine anything except his leg. She does not note that he has the multiple serious medical problems described above, including hypertension. diabetes, gout, congestive heart failure, and hyperlipidemia. as well as severe anemia. She does not refer him for a colonoscopy, an endoscopy, or for infectious disease consultation. She did request that fecal occult blood studies be checked. She wrote 'Will request chart." On June 25 there is a handwritten note nursing note: "Kite sent 'I need to know about culture sent out.' Garcia called. Lab results are being sent over today. Labs faxed per Chuck given to PA Smith." Patient #8 was never told the results of his tests. They were not in the chart I reviewed. On June 28, at 9:30 in the morning, the patient was found dead in his cell in Segregation, his pupils fixed and dilated. No attempt at cardiopulmonary resuscitation was attempted. Comment: Patient #8 was 70 years old. No autopsy was obtained. An autopsy should have been performed. Patient #8 was a 70 year old man with a severely infected swollen painful foot who was having internal bleeding. He had coronary artery disease, diabetes, hypertension, gout, and had a severe MRSA infection of his leg. He was bleeding internally, and he was allowed to die without any treatment. He should not have been discharged from Foote. When he was sent back to DWH, he should have been admitted to the Hospital, or else sent back to Foote. He should not have been sent back to the Segregation Unit at JMF to die without any medical attention to his multiple serious life threatening medical problems. This death occurred on June 28, less than two months ago. Case 4:92-cv-00110-RAE Doc:ument 1897 Filed 09/1212005 Page 52 of 60 111 3 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Coben. MD September 8. 2005 Page #51 I had met Patient #8 at JMF in his housing unit on April 21, 2004. At that time he told me that his leg was chronically and painfully swollen secondary to the saphenous vein removal that had been performed for his coronary artery bypass graft. He told he at that time that his wheelchair had been taken away from him, and that he had difficultly walking with the walker provided. When I met him his wheelchair had been given back to him. He also said that his leg and been chronically swollen since the bypass surgery, but he had not received any treatment for this problem. I brought his problem to the attention of MDOC staff at that time. Patient #9 Patient #9 had diabetes and severe hypertension. His renal function had been deteriorating during the year prior to his death in May, 2005 On March 31,2005, an urgent (ASAP) renal consultation· request was made for acute renal failure when his creatinine reached 6. slowly rising from 3.0 over the previous year. No consult had ever been provided to patient. On April 5, 2005 he had an emergency admission to Foote Hospital for uncontrolled hypertension - 200/123. He was severely hyponatremic, serum sodium was 127, creatinine increased to 6.3 and potassium was 5.9. He had emergency dialysis at Foote and an emergency fistula was placed He was discharged April 21, 2005. There is no record in the medical chart of patient receiving any dialysis after discharge from Foote. On April 29, 2005 he was seen at Endocrine Chronic Care Clinic, noted to have a blood pressure of 228/11 B and was very lethargic. according to Dr. Faghihnia. There was no treatment of this hypertensive emergency by Or. Faghihnla. He scheduled the patient for follow-up in two weeks (5/13/05). No physical exam. no fundoscopic examination, no examination of heart or lungs was performed. On that day he was sent to the DWH Emergency Room from JMF for his complaint of headache, elevated blood pressure. His blood pressure was Case 4:92-cv-00 11 O-RAE Document 1897 Filed 09/12/2005 3111 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 53 of 60 September 8, 2005 Page #52 200/110 initially, and went up to 2231113. He was treated with sublingual NTG, an then given imdur 60 mg, catapres 0.3mg, and sent back to JMF. On May 1. 2005 he was sent to the DWH ER because of a hypoglycemic reaction. He was noted to be restless. disoriented. and sweating. His blood glucose was 24 at 0408. He was given 050 (50% glucose). His blood pressure at 0413 was 184/107. At 0445 he vomited up a sandwich. At 0530 he was sent back to JMF. He was seen by nurse Charles Boltjes at 6:30 AM. His blood pressure was elevated at 169/90. The next day. his blood pressure was noted to be 201/111. He was seen by Dr. Gordon, and an evening dose of catapres 0.3rng given. No MD note was written in the chart and no follow up scheduled. The last note in the chart was written on May 4. 2005. It says his blood pressure was 180/103. COMMENT: This patient had multiple serious medical problems. He had chronic renal failure with uncontrolled hypertension and diabetes, yet received no renal consultation. His hypertension and diabetes were both very poorly controlled. yet there was no request for endocrine consultation. Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 Page 54 of 60 3"' Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD September 8, 2005 Page #53 CONCLUSIONS: There are significant problems with the care being provided to the sickest prisoners in the Hadix facilities. This is due to significant weaknesses in the provision of medical services and of specialty services. These problems were identified by the Court in its finding of 2001, and were again documented in my first and second reports. Unfortunately, these problems persist, and appear to have gotten worse over the past two years. A substantial expansion ·Df the clinical responsibility of the Hadix facilities occurred during this period, without provision of staff for the increased medical services required. The C-Unit was opened in the spring of 2003, and it currently houses approximately 64 chronically ill men who are too ill to live in general population. These prisoners often have multiple chronic illnesses, including AIDS, Hepatitis C, as well as decompensated pulmonary and cardiac illnesses. Medical staffing for this population was provided by CMS through a subcontract with the Dr. Fuller, who has been providing medical care to Duane Waters Hospital and its Emergency Room. No additional staff medical service providers were hired to care for this chronically ill prisoner population. The system of chronic care clinics, with regular structured nursing and physician evaluation according to defined protocols was not extended to this population. A large dialYSis unit, currently serving approximately 75 patients with end stage renal failure was established in JMF in 2004. These men have developed kidney failure secondary to hypertension, diabetes, AIDS, and chronic intravenous drug use. There medical problems are often exacerbated by dialysis, and they require substantial complex internal medicine care. No additional staff medical service providers were hired to address the clinical needs of this group. There has been Inadequate support by Dr. Middlebrook's nephrology group for the patients with renal failure cared for at JMF, and throughout the Hadix facilities, which need him for renal consultation. • Case 4:92-cv-00110-RAE Document 1897 Filed 09/12/2005 3ed Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 55 of 60 September S, 2005 Page #54 There is no predictable capacity for infirmary care for patients requiring intravenous medications all 24 hour nursing observation. Patient's can be admitted to Foote Hospital if they have acute needs, but Foote Hospital often sends acutely ill patients back to DWH. which sends the patients back to their sending facility - JMF, SMT, or RGC. As noted above, the medical service provider coverage for the DWH and C Unit has been extremely deficient. According to the nursing staff, and confirmed by review of medical records, nursing requests for urgent physician evaluation of serious and painful medical conditions in these units can be unanswered for days at a time, or never responded to at all (see Patient #1 below). I have never before seen a situation in which patients with complex medical problems with acute exacerbations housed in intensive medical settings are routinely denied access to physician care when specifically requested by the nursing staff. Nor have I ever imagined a situation where Nursing staff would tolerate this situation and not take appropriate action to correct the situation, and prevent it from happening again. During the past two years, there has been essentially no on-site supervision of the medical staff by eMS. Although the need for this position was identified a year ago. effectively, through April 2005, no significant supervision by provided by CMS. Although Dr. Austin was apPOinted Regional Medical Director for CMS in August. 2004, he only served in through April. 2005. CMS did not assign him to oversee the care in C-Unit until March, 2005. Dr. Austin was replaced by Dr. Matthai in April. The following recommendations are based upon my two years of work at the Hadix facilities. By design. these facilities are medically intensive. The sicker patients from throughout Michigan end up at the Jackson Medical Complex, as they should. MDOC has the responsibility of assuring that the Jackson Medical Complex can meet their medical needs. CMS bears a substantial responsibility for the current situation. They have not provided supervision for their medical staff, although they appear to be Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 31d Report of the Associate Monitor Revised and Redacted Hatfrx v. Johnson Robert L. Cohen. MD Page 56 of 60 September 8, 2005 Page #55 committed to local supervision at this time. Their staff at OWH and C-Unit has been unresponsive to the serious medical care needs of acutely ill patients, and took no significant action to address this situation. Prisoners confined in Segregation are always at the greatest risk of being denied access to necessary medical care, and physicians, physician assistants, and nurse practitioners have to be trained to take the care of these patients. At JMF there has been, and continues to be a pattern of severe neglect of these prisoners. The death of Patient #8 is particularly tragic, yet predictable based on the current attitudes towards these patients. I have noticed an unusually large number of HIV positive patients housed in segregation status. MOOC has a policy of permanent segregation for HIV positive prisoners who have been sexually active. This policy has meant that increasing numbers of III HIV positive prisoners are housed in JMF segregation, and are consequently having increasing difficulty in obtaining specialty care, as well as routine care. It is necessary that medical staff make extra effort to see their patients housed in segregation more frequently. Their patients need to be examined in a confidential setting without correction officers present. It is not possible for patients to communicate effectively when they are chained and officers are present in the room. Except in the rarest of instances, patients being examined should not be wearing chains, and physicians and other clinicians should not allow non-medical staff to be present nor patient encounters. Case 4:92-cv-00110-RAE Document 1897 Filed 09/1212005 3111 Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L Cohen. MD Page 57 of 60 September 8, 2005 Page #56 RECOMMENDATIONS Establish an acute Inflnnary capability of at least thirty beds at DWH. 1. This unit will require 24 hours nursing staffing and seven day a week MSP staffing. 2. Emergency medical coverage will be provided by the DWH ER when necessary. 3. When the unit is filled, patients requiring this level of care are to be sent to Foote Hospital. Establish a unitary medical record system 1. Assure that all laboratory studies are available in SERAPIS 2. Assure that all medications are available in SERAPIS 3. Link the SERAPIS system to the pharmacy computer system for order entry 4. Enhance the drug interaction function of SERAPISlTiny Terms to include HIV medications 5. Train and certify all nurses and MSP's in the system(s) before they begin working at the Hadix Facilities 6. Expand the SERAPIS system to include all clinical areas, specifically the Dialysis Unit, the JMF Segregation Unit, the DWH Emergency Room, DWH and C-Unit, and the Specialty Clinic Areas of DWH. 7. When Telemedicine is used on a routine basis (e.g. Dr. Hutchinson, Dr. Middlebrook) SERAPIS terminals should be available Ensure automatic renewals of all chronic medications 1. Monitor distribution of chronic medication 2. Prepare a regular study/report on medication renewals 3. Require all medications from all clinical sectors (OWH, C-Unit, Segregation, Dialysis) to be entered in SERAPIS Case4:92-cv-00110-RAE Document 1897 Filed 09/1212005 31d Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cob en. MD Page 58 of 60 September B. 2005 page #57 Define the Role for MOOC's Jackson Complex Regional Medical Director 1. Member of Jackson Medical Complex Senior Leadership Team 2. Oversight of CMS specialty consultation program 3. Oversight of CMS contract employees 4. Medical Leadership for 01 function, including audits and studies 5. Oversight of Dialysis Program 6. Oversight of C-UnitlDWH clinical complex 7. Clinical liaison to Pharmacy 8. Establish and Maintain a Continuing Education Program at the Jackson Complex Obtain Autopsy Reports of all deaths Assure that Specialty Care Services are available to all prisoners, Including those in Segregation 1. Obtain data from CMS as needed to assist in analysis of Specialty Care 2. Maintain the current MDOC Specialty Care Computer System 3. Provide MSP's with weekly lists of the status of their outstanding consults. 4. Provide handwritten consultations from to providers within twenty four hours of consultation. if dictation not available. 5. Require telephone contact by speCialists to MSP's when urgent medical information needs to be communicated. 6. CMS should not "pend" consultation while awaiting dictated consults when the consultant has written or called the MSP with specific recommendations. -I Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/1212005 3111 Report of the Associate Monitor Revised and Redacted Hsdix v. Johnson Robert L. Cohen. MP Page 59 of 60 September 8, 2005 Page #58 Develop an enhanced program of monitoring the clinical function of the Dialysis Program 1. Monthly meetings, hopefully becoming quarterly, should be held with Dr. Middlebrook, the Dialysis Administrator, JMF Leadership, designated MSP(s). Jackson Complex Regional Medical Director, and CMS Deputy Medical Director. 2. The monthly evaluation form currently in use needs to be revised and enhanced. 3. Include structured interviews with Dialysis patients as part of monthly dialysis monitoring form, and include Dialysis patients, where appropriate, at the Monthly meetings. Assure Access to Care for All Patients In Segregation 1. Maintain continuity of MSP care with assigned patients. 2. Maintain SERAPIS terminal in Segregation clinic 3. With rare exceptions, all dlnical encounters with patients in Segregation should occur confidentially, without correction staff present, while maintaining correctional staff visual observation 4. Clinical encounters in Segregation should only take place in the designated clinic area, not in "cell-side." 5. Assure that patients in Segregation have access to specialty care by having nurses verify refusals at the time of the refusal. 6. Identify the reasons for the current problem in obtaining DWH and CUnit beds for patients with chronic medical problems who should not be housed in Segregation 7. Identify other alternatives to permanent Segregation for HIV positive prisoners who are accused of sexual activity Case 4:92-cv-0011 O-RAE Document 1897 Filed 09/12/2005 3rd Report of the Associate Monitor Revised and Redacted Hadix v. Johnson Robert L. Cohen. MD Page 60 of 60 September 8, 2005 Page #59 8. Expand the current bi-monthly review of chronic care patients to include all patients in Segregation, and include interviews whenever problems are identified in chart review 9. Establish a functioning program of daily MSP rounds for all prisoners in Segregation 10. Establish a monthly meeting with mental health staff to review medical problems of severely mentally ill patients housed in Segregation. 11. Review care at RGC Segregation/Quarantine Unit and develop a plan to assure patients receive necessary medical care, including speCialty consuttations. Enhance Staffing to meet the expanded clinical responsibilities of the Hadix facilities 1. Increase staff at DWH 2. Increase staff at C-Unit 3. Hire staff for Acute Carellnfirmary Unit 4. Increase staff at JMF to cover new clinical responsibilities from the Dialysis program 5. Increase staff at JMF to adequately serve medical needs of prisoners in Segregation. Submitted September 8,2005

